COVID-19 School Resources for Managing Asthma and Allergies
- Home
- |
- Health A to Z –...
- |
- Coronavirus | COVID-19 Information
- |
- COVID-19 School Resources for Managing...
Each school year brings its own unique challenges for students with asthma and allergies. As we move through the COVID-19 pandemic becoming endemic, it’s important to know the facts.
There’s so much information and misinformation available – come to Allergy & Asthma Network for trustworthy, evidence-based guidance on COVID-19, asthma and allergies. We’ll help you navigate the school year. What’s most important? Be flexible.
The U.S. Centers for Disease Control and Prevention (CDC) offers general guidance for in-person learning at K-12 schools and early childhood settings:.
- Promote COVID-19 vaccinations and booster shots as a way to prevent severe illness.
- Consider making COVID-19 testing and vaccinations available on site as a public service. Or, connect students and school staff to off-site vaccination locations.
- Encourage students and school staff to stay home when sick with any COVID-19 symptoms. Symptoms may include fever, sore throat, fatigue, cough, shortness of breath, chills, muscle or body aches, runny or stuffy nose, nausea, vomiting, diarrhea and/or loss of taste and smell.

How can school nurses help manage COVID-19 in schools?
School nurses are trusted leaders in helping schools make decisions about their COVID-19 response. They should be involved when there’s a reported COVID-19 case at the school. Some of the activities that school nurses can help with include:
- Sharing disinfection procedures
- Implementing ventilation procedures (with consideration for students with asthma and allergies)
- Updating signs, messaging and markings that promote COVID-19 safety
- Developing appropriate care plans for students and staff who become ill
- Knowing the latest guidance from the CDC and enact the guidance as appropriate for the school setting
Are there any recommendations regarding ventilation in schools with consideration for students and staff with asthma and/or allergies?
There have been concerns related to the use of air conditioners and ventilation systems during the COVID-19 pandemic. Considerations for schools include:
- Most air conditioners recirculate air within a space – adding a filter into the HVAC system will filter out some viral particles.
- Air purifiers may help to a point.
- Regularly opened windows can bring in fresh air – be aware that this may expose students with environmental allergies to pollen and other outdoor allergens.
- COVID-19 is spread by respiratory droplets. These droplets fall to the ground within 6 feet, so social distancing remains key.
Should school staff be trained on signs and symptoms of COVID-19?
Yes, school staff should be trained on the signs and symptoms of COVID-19. They should know what to do if they suspect that they have symptoms or if a student develops symptoms while at school. Training for staff will vary by school district. Parents should feel free to contact their school district or administrator to discuss how staff is trained and to ask about the district’s procedure if a case of COVID-19 is suspected or confirmed.
How should schools handle food service during COVID-19?
The CDC offers recommendations for school nutrition staff, teachers, building managers and custodial staff to reduce the risk of spreading COVID-19 during mealtimes. These include:
- Maintain 6 feet separation between students when picking up meals and when eating.
- Improve ventilation in indoor cafeterias and eating areas, including bringing in fresh, outdoor air when possible,
- Ensure proper handwashing or use of hand sanitizer before and after eating.
- Stagger mealtimes to avoid large crowds in indoor cafeterias.
- Encourage students and food service personnel to wear a mask when picking up meals and when finished eating, especially if the community has reported high levels of COVID-19 cases.
- Increase disinfection and sanitation policies as appropriate – but keep in mind the chemicals in some disinfectants can trigger asthma. Make sure the policy takes this into account. For example, the school may want to disinfect after the school day is over.
Allergies & Asthma at School ➡
Planning for School with Food Allergies ➡
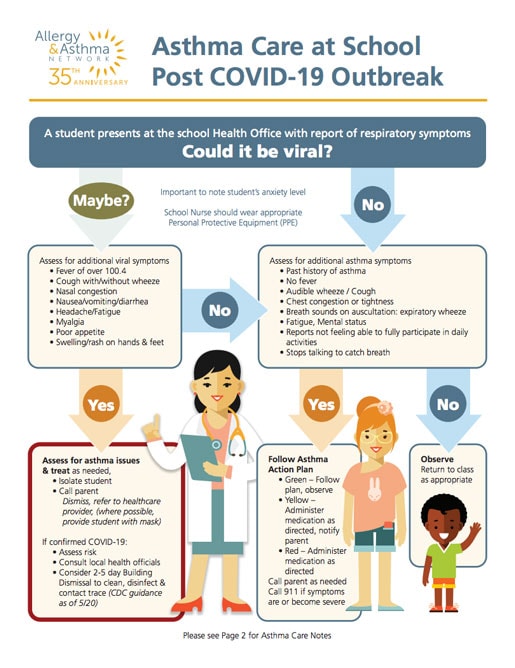
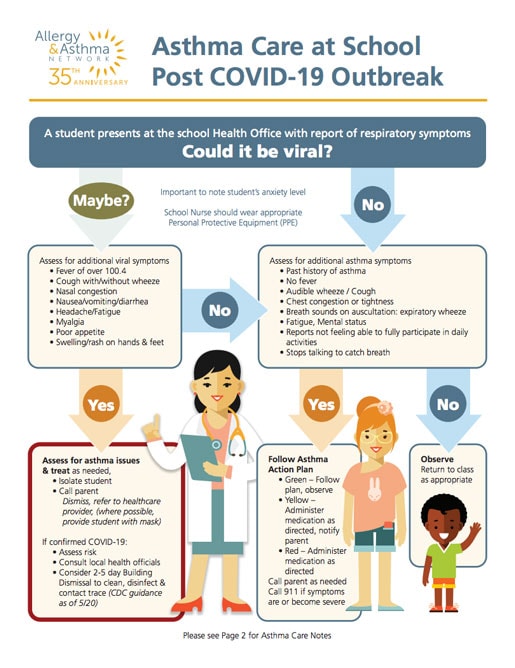
How should school health offices prepare for COVID-19?
The school should make arrangements to accommodate the isolation of a student who becomes ill with the symptoms of COVID-19 during the school day.
- Work closely with local health departments to stay updated on the latest guidance about COVID-19.
- Ensure adequate supply of face masks and PPE for school nurses, school staff and any students who may require it.
- Use vinyl or nitrile gloves. Do not substitute with latex gloves.
- Limit the number of students in the health office at one time.
- Identify isolation space and appropriate staff supervision for students with respiratory or viral symptoms.
- Develop protocols for when to isolate and dismiss students.
Are people with asthma more at risk from COVID-19?
People with moderate to severe asthma may be at higher risk of getting very sick with COVID-19, according to the CDC.
COVID-19 can affect the respiratory tract (nose, throat, lungs), which can lead to an asthma attack. It could also lead to pneumonia or acute respiratory disease. A recent study from the Journal of Allergy & Clinical Immunology demonstrated that those with non-allergic asthma may be up to 48% more at risk from severe COVID-19. The same study did not find increased risk for people with allergic asthma.
What precautions should a student or staff member with asthma take during the COVID-19 pandemic?
In addition to practicing activities to prevent COVID-19, it is crucial that people with asthma make sure their asthma is well controlled. This includes:
- Make sure you have your asthma medications and supplies (at least 30 days on hand).
- Follow your Asthma Action Plan.
- If you don’t have an asthma action plan, make an appointment TODAY to develop one with your doctor.
- Take your asthma medications as directed and don’t stop any without first discussing with your doctor.
- Know your asthma triggers and avoid them when possible.
- Know how to use your inhaler – videos are available to help.
- Learn ways to cope with stress and anxiety as strong emotions can sometimes trigger an asthma attack.
Be sure your Asthma Action Plan is up to date. Discuss any concerns with your doctor.
Should a child or staff member who is coughing from asthma and/or allergies be forced to go home?
Two primary COVID-19 symptoms are coughing and shortness of breath. These may overlap with symptoms of asthma and allergies. Students experiencing a cough and/or shortness of breath should consult with their healthcare provider before attending school.
Are disinfectants and hand sanitizers safe for students or staff with asthma?
Routine cleaning and disinfecting is key to maintaining a safe environment for faculty, students, and staff.
- Cleaning removes dirt and some germs and is generally done with soap and water.
- Disinfecting kills most germs and should be done with approved cleaning agents for the school setting.
For many students and staff, cleaning products and disinfectants are triggers for their asthma. People with asthma should try to stay away when cleaners are being used and immediately following their use.
What COVID-19 face mask policies should be in place in schools?
CDC guidelines to wear face masks are based on levels of COVID-19 in each community. The levels are determined by the total number of people with COVID-19 admitted to the hospital; hospital beds in use; and the total number of new COVID-19 cases in the area.
If a community has a high level of COVID-19, it’s recommended people wear a mask indoors in public settings, including K-12 schools. Masks do not need to be worn outside.
If a community has a medium or low level of COVID-19, face masks are based on personal preference or risk. However, for communities at medium level, people who are immunocompromised or at high risk for severe illness should talk with their doctor about wearing a mask indoors.
Check your community’s level on CDC’s website.
Some individual schools or school districts may elect to continue having students wear masks. Check with your local school for information.
Should masks be worn by people with asthma?
CDC recommends people living in a community with high levels of COVID-19 wear a face mask indoors. This includes people who are immunocompromised or at risk for severe illness, such as those with moderate to severe asthma. If the level of COVID-19 in a community is medium, people who are immunocompromised or at risk for severe illness should speak with their healthcare provider.

What are potential complications for children and COVID-19?
As a result of COVID-19, some children have experienced Multisystem Inflammatory Syndrome in Children, or MIS-C. It is a condition where different parts of the body become inflamed, including the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs.
The exact cause of MIS-C is unknown, but many children with it had COVID-19 or were around someone with it.
What are the symptoms of Multisystem Inflammatory Syndrome in Children?
- Fever
- Abdominal pain
- Vomiting
- Diarrhea
- Neck pain
- Rash
- Bloodshot eyes
- Feeling extra tired
Not all children have the same MIS-C symptoms. MIS-C can be serious, even life-threatening, but most children diagnosed with it get better with medical care.


