Food Allergies
A food allergy is an immune system response that occurs soon after a person eats a certain food. Most food-allergic reactions are mild, but some are potentially life-threatening and require emergency treatment.
What causes food allergies?
A person with a food allergy has an immune system that overreacts to proteins found in certain foods. It is identified as a dangerous invader and the body creates a specific IgE (Immunoglobulin E) antibody to fight it. This triggers a protective response that can include skin, respiratory, heart and/or digestive symptoms. Severe food allergy reactions involve two or more of these body organs.
How many people have food allergies?
Approximately 20 million Americans have food allergies – 16 million adults and 4 million children, according to 2021 data from the U.S. Centers for Disease Control and Prevention (CDC).
About 46% of adults and 40% of children with food allergies have more than one food allergen.
What are common food allergies?
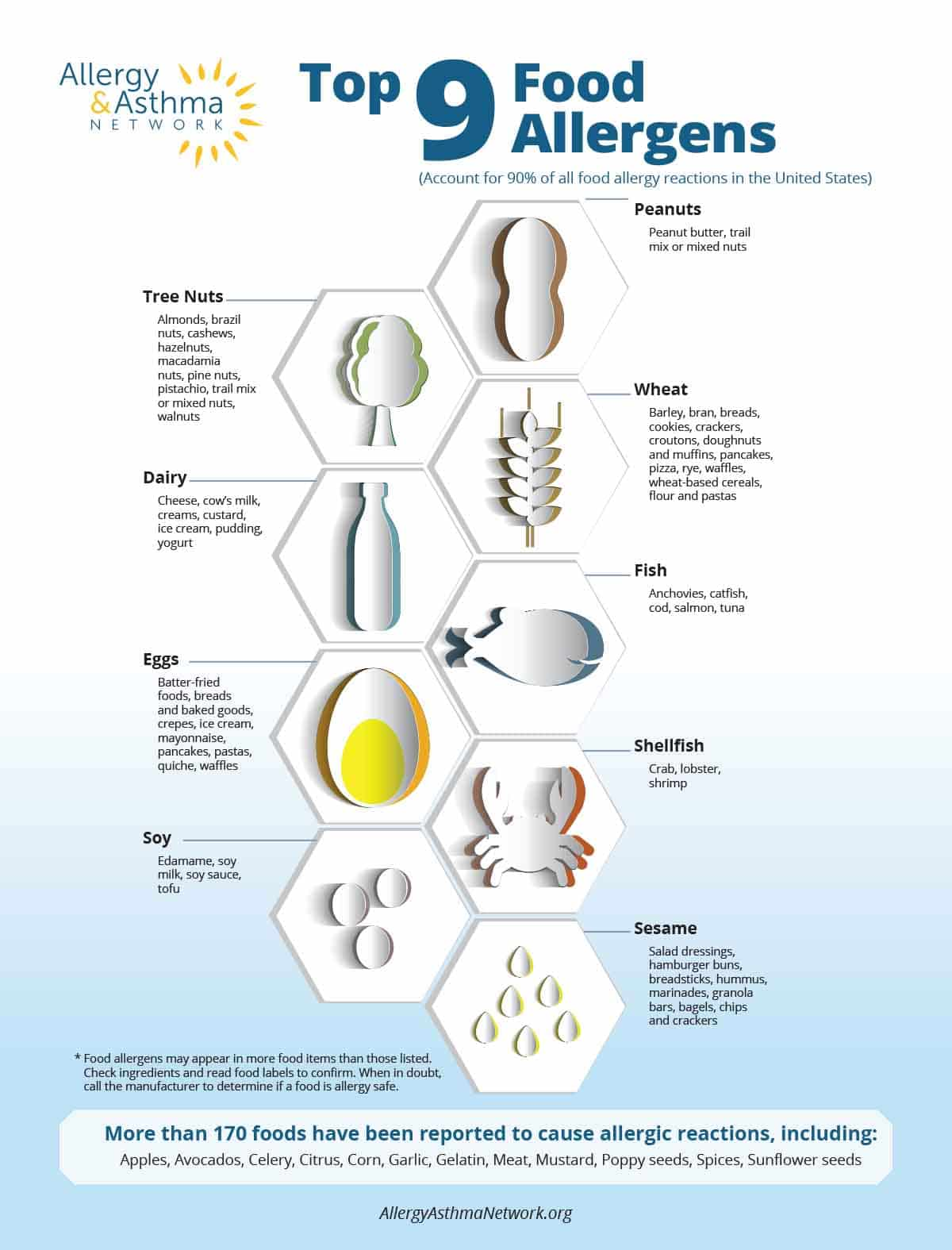
Nine foods account for 90 percent of all reactions in the United States. These nine foods are known as the “top 9” food allergies:
- cow’s milk
- eggs
- peanuts
- tree nuts
- wheat
- soy
- fish
- shellfish
- sesame
Less common food allergens include corn, garlic, gelatin, lupin, meat, mustard, poppy seeds and sunflower seeds.
What is the most common food allergy?
In infants and children, the most common food allergy is peanut, milk, shellfish, tree nuts, eggs and fish.
The most common food allergy in adults is shellfish (shrimp, crayfish, lobster), followed by cow’s milk, peanuts, tree nuts and fish (such as salmon).
What are the symptoms of food allergies?
Symptoms of food allergies can vary from person to person and from reaction to reaction.
Reactions can be different with each episode, even for the same person – that’s part of the difficulty of managing food allergies. Symptoms can range from mild to severe. Symptoms usually appear within minutes of eating the food, though they can sometimes occur hours later.
Each of the symptoms can occur alone or in combination with other symptoms. In a severe reaction, sometimes you’ll see a combination of symptoms from different body areas.
Symptoms of a mild allergic reaction are:
- Itchy or runny nose, sneezing
- Itchy or tingling sensation in the mouth
- A few hives, mild itching of skin
- Mild nausea or discomfort
Symptoms of a severe allergic reaction, also known as anaphylaxis, involve more than one body organ:
- Hives on the skin, sometimes on several parts of the body
- Shortness of breath, wheezing, repetitive cough
- Appears pale, faint, dizzy, confused
- Tightness in throat, hoarse, trouble breathing or swallowing
- Stomach discomfort such as abdominal cramps; diarrhea, or vomiting
- Swelling of tongue, lips or throat
- Blood pressure changes
- Feeling of impending doom
How is a food allergy diagnosed?
Studies show that more than half of presumed food allergies are not actually allergies. That is why an accurate diagnosis is essential.
Board-certified allergists have special training and experience in putting together to make a diagnosis of food allergy based on:
- your history of symptoms
- physical exams
- allergy testing

How can I use a food diary to track food allergy symptoms?
The first thing a doctor looks at when diagnosing food allergy is your history of symptoms. If you think you might have a food allergy, keep a written diary with the following information:
- What symptoms did you notice?
- How long after eating did you notice symptoms?
- How long did the symptoms last and how severe were they?
- Did you do anything to help ease the symptoms (such as take prescription or over-the-counter medications)?
- What exactly did you eat and how much?
- Where and how was the food processed? Was it at home? A restaurant?
- How was the food prepared: raw? boiled? roasted?
- Were you doing anything else during or just after your meal, like exercising?
Show your diary to your doctor. Sometimes the food allergy is obvious, but follow-up testing is important to confirm the diagnosis.
Ask the Allergist with Priya Bansal, MD: Should a child with eczema be tested for food allergy?
What kinds of tests are done for food allergies?
The food allergy tests performed most often by allergists are:
- skin prick test
- blood test
- oral food challenge
Skin prick tests
A diluted extract of the food is placed on your skin, then the skin is scratched with a needle. If you develop a raised skin reaction (called a wheal) at the place of the needle prick, that indicates possible allergy. If there is no reaction, you are unlikely to be allergic to the food.
Skin prick tests are quite accurate for foods with stable proteins, including peanut, milk, egg, tree nuts, fish and shellfish – some of the most common food allergens in the United States. They are less reliable for fruits and vegetables, which have proteins that break down quickly.
Blood tests
Blood tests that look for IgE antibodies are useful for identifying food allergies. They are particularly helpful for people whose allergy history puts them at high risk of serious reaction to a skin prick test; whose skin problems make skin-prick uncomfortable or dangerous; or who take certain medications that interfere with skin prick test results.
Oral food challenge
Your doctor may recommend an oral food challenge test to diagnose a food allergy. The patient is asked to eat very slowly a tiny amount of a food, then gradually larger amounts, to determine if there’s an allergic reaction.
Because an oral food challenge always carries risk, it should be performed by an allergist trained in how to conduct the test and at a medical facility that has epinephrine, oxygen, IV fluids and other treatments for potentially severe reactions.
Food challenges are safe when done properly – only about 2% of people experience anaphylaxis from testing.
Testing with large panels of food allergens is not recommended
Allergy experts do not recommend using food allergy panel blood testing. Panels test many different foods all at one time. Panels are not recommended because allergy blood tests are not entirely accurate.
Blood tests may have what is known as false positive results, where a test for a food allergy is positive but the person is not truly allergic. This is why allergy testing alone cannot be used to diagnose a food allergy.
Patients who test “positive” to numerous foods might choose to eat very restrictive diets, which can be unhealthy and difficult to follow. That’s why seeing an allergist trained to put all the evidence together for a diagnosis is important.
How do I treat a food allergy reaction?
If you experience a mild reaction that involves just one body system, follow your doctor’s instructions for treatment. You may only need to take an antihistamine like Benadryl® if you just develop hives, for example. However, keep in mind that mild symptoms can quickly become severe and turn into anaphylaxis. Skin symptoms like hives are not always present with anaphylaxis.
For anaphylaxis, epinephrine is the first line of treatment. In a severe reaction, do not delay treatment – treat with epinephrine IMMEDIATELY. Treating anaphylaxis in the first few minutes can save a life.
Epinephrine is the only treatment that can stop or slow anaphylaxis. Antihistamines will have limited to no effect treating a severe allergic reaction.
If you’re not sure the symptoms are anaphylaxis, give epinephrine anyway. Epinephrine is generally safe and effective, even if given when not needed. It can cause side effects such as anxiety, dizziness, shakiness, headache, and nausea, but these are usually mild and not life-threatening.
GIVE EPINEPHRINE FIRST, GIVE EPINEPHRINE FAST
If your anaphylaxis symptoms go away after one dose of epinephrine and you feel better, you may not need to seek emergency medical care. However, if you have severe anaphylaxis, if symptoms do not go away promptly or completely, or if symptoms return or worsen, you should take a second dose of epinephrine and seek emergency medical care.
People at risk for anaphylaxis are advised to always carry two doses of epinephrine. Some people may experience a second reaction after the first dose of epinephrine is given. This is called a biphasic reaction. If this occurs, or symptoms worsen after the first dose, take the second dose and seek emergency treatment.
Most food allergies are serious. Schedule regular checkups with your allergist to update your treatment plan.
Can a food allergy go away?
Some children will outgrow their food allergies over time, particularly if they are allergic to milk, egg or wheat. It is less common to outgrow an allergy to peanuts or tree nuts, although it is still possible.
There is now an FDA-approved oral immunotherapy (OIT) treatment for peanut allergy available for children ages 1-17. For other food allergens and/or age groups, talk with a board-certified allergist who specializes in OIT.
In OIT, patients are given the food to which they are allergic. The treatment starts with a tiny dose of the allergen and then gradually larger amounts so the body builds up tolerance to it. OIT should only be done under a doctor’s supervision. Do NOT try it on your own.
Learn more about peanut allergy OIT on our Peanut Allergy Treatment page.
Another peanut allergy immunotherapy option coming soon is the peanut patch. This is a small patch containing a dose of peanut protein that is applied to the patient’s skin daily. The therapy aims to desensitize immune cells in the skin. This makes the body more accepting of peanut in case of an accidental exposure.
Are food allergies genetic?
Why are food allergies on the rise?
Researchers don’t know for sure why allergy rates are increasing, but they are working hard to find out.
One theory is that parents for years avoided introducing common food allergens – such as peanuts or tree nuts – and that when children were introduced to these foods at an older age, their immune system overreacted. Researchers now believe that eating common food allergens at an early age can train both the immune system and the gut to tolerate these foods.
Similarly, another theory called the “hygiene hypothesis” suggests that living conditions in much of the world might be too clean and children are not fully exposed to enough germs (or microorganisms) that train their immune system (including the gut microbiome) to tell the difference between harmless and harmful substances, including foods.
Another theory suggests that children may not be exposed to enough Vitamin D (or sunlight), especially early in life. Studies show exposure to Vitamin D can help our immune system better regulate itself, develop a healthy response to foreign substances and make us less susceptible to allergies.
How can I prevent food allergy reactions?
The only proven way to prevent an allergic reaction is to avoid foods to which you are allergic.
It’s important for people with food allergies to always be thinking about how to avoid risk and prevent an allergic reaction. Here are some important ways to prevent a reaction:
- Talk with your doctor about how to prevent exposures to the foods you are allergic to.
- Read labels every time before you eat a food to make sure it’s safe for the allergies you manage.
- Make sure you use caution when choosing foods while away from home and when dining out in restaurants. Ask about ingredients, including how meals are prepared and served.
- Do some advance planning to travel safely with food allergies.

How can I be prepared to treat a food allergy reaction?
It is very important to always be prepared to treat a food allergy reaction. Never leave home without epinephrine – even if you do not plan to eat where you are going. Accidental exposures are never planned.
Make sure you know how to administer your epinephrine product. Several devices are on the market, including different types of auto-injectors and the nasal spray. Drug manufacturers have trainers you can use to practice taking the medication.
And make sure all caregivers and family members know how and when to administer epinephrine in an emergency.
Have an anaphylaxis care plan
Ask your doctor for a written Anaphylaxis Care Plan and give that to your family members, supervisor at work, your child’s school and all caregivers.
Always have epinephrine nearby
Be sure to keep two doses of epinephrine with you to use in an emergency. Epinephrine should be stored at a temperature between 68 – 77 degrees F. The epinephrine nasal spray neffy® can be kept at temperatures of up to 122 degrees for a brief period of time, but not long-term.
Think about your storage options and what works best for you. Keeping it in the glove compartment of the car may be too far away, or too warm or cold for storage.
There are several forms of epinephrine available on the market. The injector and nasal spray. Be sure you know how to use your epinephrine.
Make sure all caregivers and family members know how to use your specific epinephrine injector or nasal spray.
Wear a medical alert bracelet
Consider wearing a medical alert bracelet that lists the foods you’re allergic to and has instructions to administer epinephrine if you are unable to do so.
How can I prevent my baby from having food allergies?
How do I introduce peanut into my baby’s diet?
Living with Food Allergies
Living with food allergies is an adjustment and will require you to make some changes to your home, how you prepare foods, and how you interact with others. Someone with a food allergy can do just about anything except to eat the food to which he is allergic. However, you will need to plan in advance and communicate clearly and calmly to others to be successful.
Examples of day-to-day living that need to be planned for include:
- reading labels
- avoiding cross contact
- sending a child off to school or daycare
- using babysitters or caregivers
- ordering takeout food, like coffee
- playdates
- social gatherings and celebrations
- dining out
- traveling
How do I dine out with food allergies?
Allergists recommend the following to dine out safely:
- Call the restaurant ahead of time or check menus online before eating out.
- Communicate with the restaurant staff about your food allergies. Create a chef card that lists your allergies and ask that it be given to the chef or kitchen staff.
- Read menus closely and don’t order foods likely to cause an allergic reaction. Ask about ingredients.
- Carry two doses of epinephrine in case you experience a severe anaphylactic reaction.
Establish an open dialogue with everyone at the restaurant – the manager, host, servers and even the chef. This can help ensure you receive a safe meal. The more you talk with the restaurant staff, the more you can develop an intuition whether the restaurant is a safe place to dine. For example, if the restaurant staff confuses your food allergy with a gluten-free meal, that may be a red flag.
Establish an open dialogue with everyone – the manager, host, servers and even the chef – to ensure you receive a safe meal. The more you talk with the restaurant staff, the more you develop an intuition whether the restaurant is a safe place to dine. For example, as you speak to the restaurant staff and they seem to be confusing your food allergies with a request for a choice of a gluten-free meal, that’s a red flag.

How do I send my child off to school with food allergies?
What are other types of reactions to foods?
There are other types of reactions to foods which are different than an IgE-mediated food allergy that can cause anaphylaxis. The symptoms, diagnosis and treatment can vary depending upon the condition. Here are some of them.
Oral Allergy Syndrome
Oral allergy syndrome (OAS) is also known as pollen-food allergy syndrome. OAS happens when people with pollen allergies to certain trees, grasses and weeds develop symptoms when they eat botanically related fruits and vegetables. Usually , OAS results in mild allergy symptoms, but symptoms may get worse during pollen season.
As many as one out of every three people with seasonal allergies may experience oral allergy syndrome. The exact number is unclear because the condition often goes undiagnosed. Symptoms can be mild and go away quickly, making it less likely that people will see a doctor for diagnosis. Or parents might not associate a child’s dislike of a vegetable with an allergic reaction.
FPIES
Food protein-induced enterocolitis syndrome, or FPIES, is a severe type of food reaction that affects infants and young children – but it is not similar to food allergies.
FPIES is a non-IgE-mediated reaction to a food protein. Symptoms occur in the gastrointestinal system. FPIES causes vomiting and dehydration that can lead to shock in very severe reactions.
Eosinophilic Esophagitis
Eosinophilic esophagitis (EoE) is a chronic condition that occurs when an increased number of inflammatory cells called eosinophils cause swelling in the esophagus, making it difficult to swallow. In some people, EoE can be triggered by a food allergen or by environmental allergens such as pollen and mold. But doctors and researchers are not sure what causes it.
Celiac Disease
People with Celiac disease are unable to eat foods containing gluten, a protein found in wheat, barley and rye.
Celiac disease is an autoimmune disease. It is not an allergy or food intolerance. People with Celiac disease do not go into anaphylactic shock if they eat gluten-containing food. Instead, the body’s immune system attacks healthy cells in the intestines, causing a reaction that is sometimes severe and immediate.
This can severely damage the lining of the small intestine and lead to debilitating symptoms. The condition impacts both children and adults. It is more common among Caucasians and more diagnosed in females.
Food Intolerance
A food intolerance involves the digestive system. Due to an enzyme deficiency or chemicals in the food, the meal is not “broken down” correctly in the body and causes stomach distress. With a food intolerance, you may be able to eat small amounts of the food but have problems when you eat a lot of the food.
The most common food intolerance is to lactose intolerance. Lactose is a sugar found in milk and other dairy products. Some people are intolerant of sulfites or food additives.
Alpha-Gal Syndrome
People can be allergic to meat – specifically red meat such as beef, pork or lamb – but only under certain conditions. Commonly called red meat allergy, or alpha-gal syndrome after the blood carbohydrate involved in the allergy, the condition is connected to a recent tick bite.
The tick transfers the alpha-gal sugar molecule to the host, causing the allergy to develop. Symptoms occur after eating red meat and are similar to other food allergy symptoms, but with more gastrointestinal distress. Red meat allergy is also referred to as mammalian meat allergy, lone star tick disease or tick bite meat allergy











