Food Allergy Treatment & Management

Approximately 20 million people live with food allergy in the United States. This includes about 16 million adults and 4 million children. Food allergy is caused by the immune system reacting to specific foods. Allergic reactions can range from mild to life-threatening.
If you have a food allergy, then food allergy prevention and preparedness are part of your daily routine. It’s important to know how to manage food allergies and know how to treat an allergic reaction. Learn more about food allergy causes, symptoms, and diagnosis.

Treatment for food allergies
There is no cure for food allergy. If you have a food allergy, you need to be prepared to treat a severe allergic reaction should one occur. The treatment for a severe allergic reaction, or anaphylaxis, is epinephrine.
Your allergist may recommend food allergy oral immunotherapy (OIT). This is a specialized treatment that can help your body build tolerance to your food allergen. This makes it less likely an allergic reaction will occur due to an accidental ingestion.
An FDA-approved oral immunotherapy treatment for peanut allergy is available. It is called Palforzia™. Many allergists now also offer office-based oral immunotherapy for peanut and other food allergens.
A biologic medication is available as a food allergy therapy. FDA has approved omalizumab (Xolair®) for people with food allergies. It helps them to tolerate an accidental exposure to a food allergen. It also reduces the risk of an allergic reaction.
What is the first-line treatment for a severe food allergy reaction?
Epinephrine is the first-line treatment for a severe or life-threatening allergic reaction, or anaphylaxis. In most cases, symptoms of anaphylaxis involve two or more body organs (skin, respiratory system, digestive system, heart).
If you have severe food allergies, it’s best to carry epinephrine with you. If you experience anaphylaxis symptoms, administer epinephrine right away. Don’t try to wait it out. Administer epinephrine first and fast. The medication may not be effective if you wait too long to use it.
Make sure you carry two doses of epinephrine with you at all times, as sometimes symptoms can return after the first dose. Know when and how to administer epinephrine. Make sure the medication is not expired. Get refills if needed.
If your anaphylaxis symptoms go away after one dose of epinephrine and you feel better, you may not need to seek emergency medical care. However, if you have severe anaphylaxis, if symptoms do not go away promptly or completely, or if symptoms return or worsen, you should take a second dose of epinephrine and seek emergency medical care.
What if your symptoms are mild? Do you need to use epinephrine then? No. You should administer epinephrine if symptoms involve two or more body organs and are severe or worsening. For symptoms that are mild and involve just one body organ, such as an itchy mouth (oral allergy syndrome) or a runny nose, your doctor may recommend an antihistamine.
When you next meet with your doctor, make sure to discuss your treatment plan and review food allergy treatment guidelines.

What is food allergy oral immunotherapy (OIT)?
Food allergy OIT is relatively new. It starts with giving a tiny amount of the food allergen, then gradually larger amounts until a target dose is reached. This helps desensitize the patient should they have an accidental exposure to their allergen triggers.
Food allergy OIT should only be done in a medical setting such as an allergist’s office. Do NOT attempt oral immunotherapy on your own. It involves having the food allergic person eat increasing amounts of their allergen. This starts in very small amounts and gradually increasing over a period of months.
The only FDA-approved oral immunotherapy is for peanut allergy. It is called Palforzia™. This treatment is for children ages 1-17. It is not meant to cure peanut allergies. Rather, it is to help reduce the frequency and severity of peanut allergy symptoms in case of an accidental exposure.
What about immunotherapy for cow’s milk allergy, egg allergy, or other food allergens? Researchers are studying immunotherapy for these allergens. But there are no FDA-approved options at this time.
Allergists who specialize in food allergy may offer an office-based oral immunotherapy treatment. These may treat peanut and other types of food allergens. These are not FDA-approved, however. While office-based immunotherapy is not FDA approved, many people with food allergies have successfully been desensitized to their food allergen(s) through this approach.
Researchers are also studying oral immunotherapy to treat people with multiple food allergies using biologic medications.
What is biologic therapy for food allergy?
In February 2024, FDA approved omalizumab (Xolair®) as a food allergy therapy. The biologic medication targets and blocks the Immunoglobulin E (IgE) antibody. IgE is a driver of food-allergic reactions. Reducing IgE levels keeps the body from reacting to an allergen.
Xolair is an added layer of protection against an allergic reaction. It allows people with food allergies to tolerate an accidental exposure to a food allergen. It also reduces the risk of an allergic reaction.
Xolair is approved for adults and children ages 1 year and older with food allergy. It is taken as an injection every 2-4 weeks. Patients can receive the injection in a healthcare setting. They can also self-inject it at home if approved by their healthcare provider.
It is important to remember that Xolair is not a food allergy cure. People taking the medication as a food allergy therapy must continue to avoid their food allergen(s). They should also continue to carry and use epinephrine in case of a severe allergic reaction.
Managing food allergies
If you have recently been diagnosed with food allergy, you may feel uncertain or cautious about what you can eat. Severe allergic reactions can be severe and life-threatening. Food allergy is serious, and it is important to take an active role in managing it.
How do you prevent an allergic reaction?
You can prevent food allergies by avoiding your known food allergen(s). The first thing you need to do is know which food(s) cause an allergic reaction. When you understand what foods to avoid and how to identify them on food labels, you take a step forward in managing your food allergy.
Keep track of your symptoms. Write down in a diary what meals you ate and whether foods caused any allergy symptoms. If you experience allergy symptoms to a food, make an appointment with a board-certified allergist for testing. Food allergy testing may include a skin prick test, blood test or an oral food challenge. Your allergist will diagnose food allergy based on the test results, your symptoms, and your medical history.
Once you know your trigger food(s), develop a plan to avoid those foods. Sometimes, even with your best efforts, you may have an accidental exposure to your food allergen. If you’re at risk for a severe allergic reaction, you will need to treat it with epinephrine.
Foods to avoid
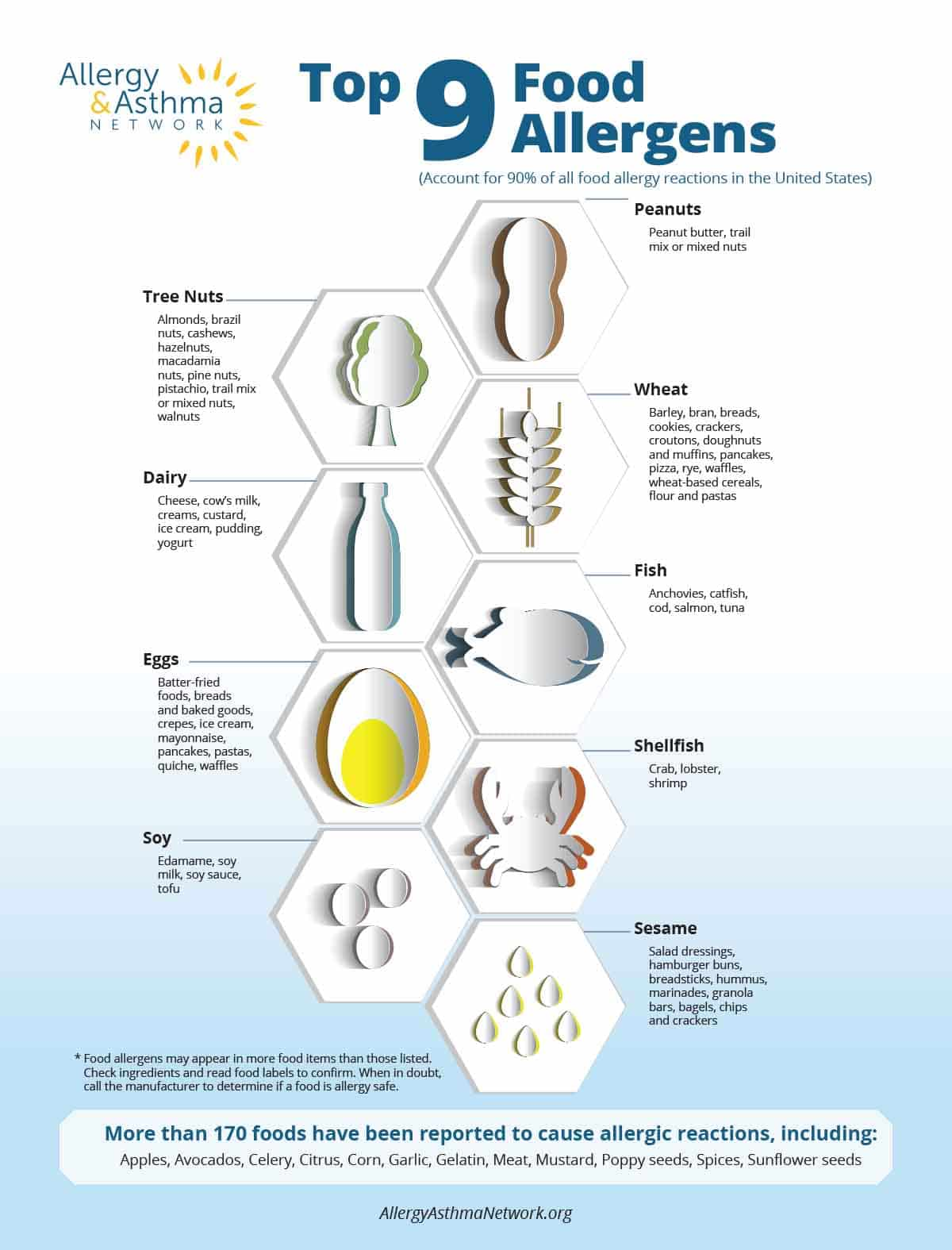
Nine foods account for 90% of all food allergies. These are:
- cow’s milk
- eggs
- peanuts
- tree nuts (almonds, cashews, pistachios, pecans, walnut, hazelnut, etc.)
- wheat
- soy
- fish (includes bass, trout, cod, salmon)
- shellfish (lobster, shrimp, crab)
- sesame
When you’re allergic to a food, it’s important to know what types of foods contain your allergen. Learn ingredients and check food product labels to ensure you avoid your food allergen.

Reading food labels
The Food Allergy Labeling and Consumer Protection Act (FALCPA) requires food manufacturers to label if their product contains one of the nine most common food allergens. These are milk, egg, wheat, soy, peanut, tree nut, fish, crustacean shellfish and sesame. Food manufacturers must list allergens in clear, plain language. The listing must be part of the ingredients and in a “Contains” statement placed immediately after the ingredients.
The law applies to any food flavoring, spice, food coloring or processing aid that contains a Top 9 allergen. The law does not apply to meat or poultry and gluten-containing grains other than wheat. Molluscan shellfish such as clams, oysters, mussels and scallops are not considered a major food allergen under the law.
Food manufacturers are not required to list highly refined peanut, tree nut or soy oils. The processing of these products separates the allergen protein from the oil. So they are considered safe.

Some tips for reading food labels:
- Check food labels when shopping for groceries. First, look for the “Contains” statement on the food label. If your allergen is listed, put the product back on the shelf.
- If there’s no “Contains” statement on the food label, check the ingredients list to see if your allergen is present. If it is, put the product back on the shelf.
- Make sure you know all your food allergens and the different ways they may be listed. Ingredients derived from common food allergens can be listed under many different names.
- Avoid foods with advisory statements on allergens, such as “May contain…” or “Produced in a facility that…” or “Manufactured on shared equipment…” This means there’s a chance your food allergen is present in the product. It could have been made using equipment that made other foods containing your allergen.
- If you have a less common food allergy, work with your allergist or a dietician to understand any and all ingredients to avoid.
- Read every label, every time, even if a product you bought previously was a “safe” food. Food manufacturers can change ingredients of products without notice.
- If you are unsure about whether a food contains your food allergen, don’t buy it. Check with the manufacturer to be sure.

Avoiding Cross-Contact
When an unsafe food allergen comes into contact with a food that’s safe for you, this is called “cross-contact.” It happens more often than you think. Cross-contact could occur from dipping a knife in the jelly jar after using it to spread peanut butter. Or it could happen after using the same grill or pan to cook a hamburger after it was just used to cook shellfish. Or cross-contact might happen after chopping almonds on a cutting board and then slicing a tomato.
Here are some tips to avoid cross-contact:
- Wash hands in soap and water before preparing a meal. Commercial hand wipes are also effective; studies show hand sanitizers are not.
- Wash cutting boards, dishes, pots, pans and countertops thoroughly with hot, soapy water after preparing food items.
- Cook the allergen-safe meal first to minimize risk.
- Designate a separate shelf in the refrigerator and cupboard for allergen-safe foods. Use stickers to identify them as “allergen safe.”
- At restaurants, ask that your food be prepared in a separate cooking area with clean and separate pans and utensils. This includes deep fryers.
- Never share food, utensils or drinks.
- Avoid buffets or cafeterias, which have a greater risk of cross-contact due to shared utensils and spilled foods.
Anaphylaxis Emergency Action Plan
An important part of managing food allergies is to have an emergency treatment plan in place. An Anaphylaxis Emergency Action Plan is a written care plan outlining treatment for a severe or life-threatening allergic reaction. The action plan should include:
- Your name and age
- Your allergies or trigger food
- Emergency medications and instructions for using them
- Directions to call 911
- Emergency contacts
Carry the action plan with you at all times so you and others know what to do in case of anaphylaxis.
- Emergency action plan for adults – AAAAI (PDF)
- Emergency action plan for children – AAP (PDF)
- Food allergy & anaphylaxis emergency care plan in English – FARE (PDF)
- Food allergy & anaphylaxis emergency care plan in Spanish – FARE (PDF)

Shared Decision-Making (SDM) and food allergies
Shared decision-making is a strategy for patients and their doctors to partner together when making decisions about management and treatment. Discuss the risks and benefits of treatment. Understand the time commitment. This way you are better informed to make the right decision for your health. You’re also more invested in following the treatment plan.

Managing food allergies in children
Approximately 4 million children live with food allergy in the United States. Food allergy is more common in children ages 12-17 than younger children. Black, non-Hispanic children are more likely to have food allergies than non-Hispanic White and Hispanic children.
Recognizing food allergy symptoms in young children
Babies and young children are unable to communicate their food allergy symptoms. So it’s important that parents and caregivers know what symptoms to watch for so they can identify a food allergy.
Symptoms of food allergy in infants and young children include:
- Difficulty breathing, coughing or wheezing
- Difficulty swallowing
- Itchy hives on the skin
- Swelling on lips, tongue or mouth
- Nausea or vomiting
- Cramping or diarrhea
- In severe cases, a drop in blood pressure
Young children may also become very tired or lethargic due to a food allergy. Some may become very irritable.
If you notice any of these symptoms in your child, seek medical care right away.
It’s also important to note that severe eczema is a risk factor for peanut allergy in children. If your baby or young child has severe eczema, talk with a board-certified allergist about food allergy testing.
Common food allergies in children
Eggs, cow’s milk and peanuts are the most common food allergies in children. Wheat allergy, soy allergy and tree nut allergy are also common.
For many years, doctors recommended parents wait before introducing common food allergens foods to babies and infants. Research now tells us that early introduction of food allergens – particularly peanut – may help prevent food allergies.
Current food allergy guidance recommends introducing peanut as early as 4-6 months of age. This is especially the case if the child has severe eczema. The baby should first see an allergist for allergy testing. This will help determine if peanut can be safely introduced, and if it needs to be done in a doctor’s office.
Important: Parents of children at risk for food allergy should not introduce that food into their child’s diet without first consulting an allergist who can closely supervise and monitor the results.

Managing food allergies in adults
Approximately 20 million adults live with food allergy in the United States. Food allergy is more common in women (7.8%) than men (4.6%). Black, non-Hispanic adults are more likely to have food allergies than Hispanic, non-Hispanic White, and non-Hispanic Asian adults.
Challenges faced by adults with food allergies
Adults face unique challenges living with food allergies. Work or social events, family get-togethers, travel and dining out increase risk of accidental exposure.
It’s important to not become complacent when managing most food allergies. Stay vigilant in avoiding your trigger food. Studies have found that adults are less likely to have an up-to-date prescription for epinephrine as they get older.
Managing food allergies in social situations
From office potlucks to holiday get-togethers to special events, food is often the way we socialize. If you live with a food allergy, you may feel anxiety attending these social occasions. Here are some tips to help you feel safe:
- Offer to host events yourself and limit the amount of food brought from others in attendance.
- Make sure your family, friends and colleagues are aware of your food allergy.
- Bring one or two allergy-safe dishes that you prepared yourself.
- Carry a chef’s card with you when dining out. Give it to servers, cooks and/or the chef prior to ordering to alert them about your allergy. Or you can give to a family member or friend when eating at their house.
- Always carry epinephrine with you.
Recently diagnosed with a food allergy?
You may feel anxious or overwhelmed. This is, after all, a life-changing diagnosis. Once you identify your trigger food, you can learn to avoid your allergen and prevent an allergic reaction. And if an accidental exposure occurs, you can learn what to do to keep symptoms from becoming life-threatening.
Check out our Living with Food Allergies page to learn more!
Questions & Answers (Q&A) on Food Allergy Treatment & Management
You may have specific questions about how to treat an allergic reaction or manage your food allergy. Here’s a Q&A with some common questions about food allergies and anaphylaxis. If there’s another topic you would like to see addressed, please email our editor.
Other conditions that may look like food allergies or co-exist with food allergies?
There are other conditions that are different than food allergies but the symptoms, diagnosis and treatment vary depending upon the condition. Here are some of them.
Reviewed by…
Purvi Parikh, MD, FACAAI, is an adult and pediatric allergist and immunologist at Allergy and Asthma Associates of Murray Hill in New York City. She is on faculty as Clinical Assistant Professor in both departments of Medicine and Pediatrics at New York University School of Medicine.
Michael Pistiner, MD, MMSc, FACAAI, is a board-certified pediatric allergist and immunologist. He serves as the Director of Food Allergy Advocacy, Education and Prevention of the Food Allergy Center at MassGeneral Hospital for Children in Boston. He is the co-creator of the allergy educational website AllergyHome.org.










