What is Eczema?
Eczema is a very common skin condition. Eczema is not a single condition, but rather a grouping of several types of skin conditions, not all of which are related to each other.
How common is eczema?
Eczema is a skin condition that affects 31.6 million people in the United States. Atopic dermatitis is the most common form of eczema; 16.5 million adults and 9.6 million children under the age of 18 have atopic dermatitis. Among children, 3.2 million have moderate-to-severe symptoms. Eczema often develops in early childhood, appearing within the first 6 months or within the first 5 years.
What causes eczema?
The cause of eczema is unknown, but doctors believe that it is related to genetics, an immune system that is sensitive to allergens and irritants and a defective skin barrier that allows moisture to escape and allergens and bacteria to invade. Approximately 70% of people with eczema report a family history of the condition.
Exposure to allergens and irritants start a chain reaction in the body. The immune cells release histamines, cytokines and other chemicals to get rid of the irritants. The resulting inflammation causes the skin to itch, and itch and itch.
Too much scratching can lead to infection if the surface of the skin is broken. Signs of an infection include yellowish, crusty skin (often on top of the eczema), red, swollen bumps and pus-filled blisters.
Some people with eczema may lack a specific type of protein, called filaggrin, in their skin. This protein serves as a protective barrier from allergens, irritants and infections. When filaggrin is lacking, it weakens the skin barrier function of the skin. Some people with eczema also have high blood levels of Immunoglobulin E, or IgE, which are antibodies produced by the immune system that set off allergy symptoms.


Get a Free "Understanding Atopic Dermatitis" Guide ➤
Understanding Atopic Dermatitis (English Version)
Entender la Dermatitis Atópica (Versión en español)

What are the different types of eczema?
There are seven different types of eczema. Each type has its own unique triggers and causes. Treatment options may vary depending on the type of eczema a person has. Let’s look at the different types of eczema.
1. Atopic dermatitis
Atopic dermatitis is a chronic inflammatory skin condition. It is the most common type of eczema. You may often see atopic dermatitis used interchangeably with eczema, even though it is only one type. It affects 16.5 million adults and 9.6 million children. Atopic dermatitis has a genetic component as it tends to run in families.
With atopic dermatitis, the immune system is easily triggered and sensitive to allergens and irritants. Many people with atopic dermatitis also have a mutation to the filaggrin gene, causing them to have a compromised skin barrier. This, along with inflammation that can damage the skin, allows for moisture to escape and allergens and bacteria to invade.
Symptoms may come and go. They include:
- Red, itchy patches of skin on light skin; dark brown, purple or ashen gray on dark skin
- Dry and scaly skin
- Areas of thickened skin
- Open, oozing, and crusty sores.
People with atopic dermatitis often also have other allergic conditions such as asthma or allergic rhinitis.
2. Dyshidrotic eczema
Dyshidrotic eczema is another common form of eczema. It causes small, itchy, fluid-filled blisters to form on the hands and feet as the result of an allergic response. It tends to run in families. Dyshidrotic eczema is seen in people with other types of eczema and it is more common in women than men. It rarely appears in children under 10.
3. Contact dermatitis
Unlike many other types of eczema, contact dermatitis doesn’t run in families. With contact dermatitis, the skin becomes irritated when it encounters an allergen or irritant.
There are two subtypes of contact dermatitis: allergic or irritant.
- Irritant contact dermatitis – this is the most common type of contact dermatitis. The skin becomes damaged due to contact with an irritant such as a cleaning product (detergent, soap), makeup or certain metals. It can also occur from the skin rubbing against scratchy clothing.
- Irritant contact dermatitis – this is the most common type of contact dermatitis. The skin becomes damaged due to contact with an irritant such as a cleaning product (detergent, soap), makeup or certain metals. It can also occur from the skin rubbing against scratchy clothing.
4. Neurodermatitis
Neurodermatitis affects approximately 12% of the U.S. population. Whereas atopic dermatitis tends to be widespread across the body, neurodermatitis is normally confined to one or two patches of skin. The most common areas affected are arms, shoulders, elbows, legs, ankles, wrists, hands, back of the neck or scalp. These patches of skin can be dry, thick, scaly, leathery or different colored. They are very itchy.
Neurodermatitis is more common in women than men. Many people report the itchiness being worse when trying to relax, such as at bedtime, or during periods of high stress.
5. Nummular eczema
People with nummular eczema develop coin-shaped patches of skin that are itchy and may ooze. These areas often develop on arms, legs, hands, or torso. They itch and burn, and fluid may leak out and crust on the skin. The condition is more common in males than females. It can be seen independent from other types of eczema or at the same time.
6. Seborrheic dermatitis
Seborrheic dermatitis is a skin condition most common on the scalp. It also occurs in other areas with lots of oil gland activity. Seborrheic dermatitis is characterized by red, itchy, scaly and greasy patches of skin which produce flaking. It is commonly known as dandruff in adults and teens or cradle cap in infants.
Approximately 11% of the U.S. population has seborrheic dermatitis. It is common in people with certain medical conditions such as adult Hodgkin’s lymphoma, HIV, Down syndrome and Parkinson’s disease.
7. Stasis dermatitis
Stasis dermatitis occurs in people with poor circulation (venous insufficiency) to their lower legs. It is most common in older adults and women. Common risk factors for developing poor circulation include varicose veins, high blood pressure, obesity and heart failure.
People with stasis dermatitis often start with ankle swelling and orange-brown spots. \ It may also lead to skin color changes, itching, scaliness and dry skin.
So eczema is a versatile disease. Each type has different causes and manifestations. It is important to work with an allergist or dermatologist (skin doctor) for treatment. Depending on your type of eczema, you may need to also work with other specialists to help treat conditions that may be contributing to your eczema.
What are common symptoms of eczema?
Eczema can come and go, but even when skin appears clear, there may be inflammation under the surface of the skin, waiting to flare.
Common signs and symptoms of eczema include:
- itching
- flaking
- cracking
- swelling
- open oozing skin
- crusting
- dry skin
- sensitive skin
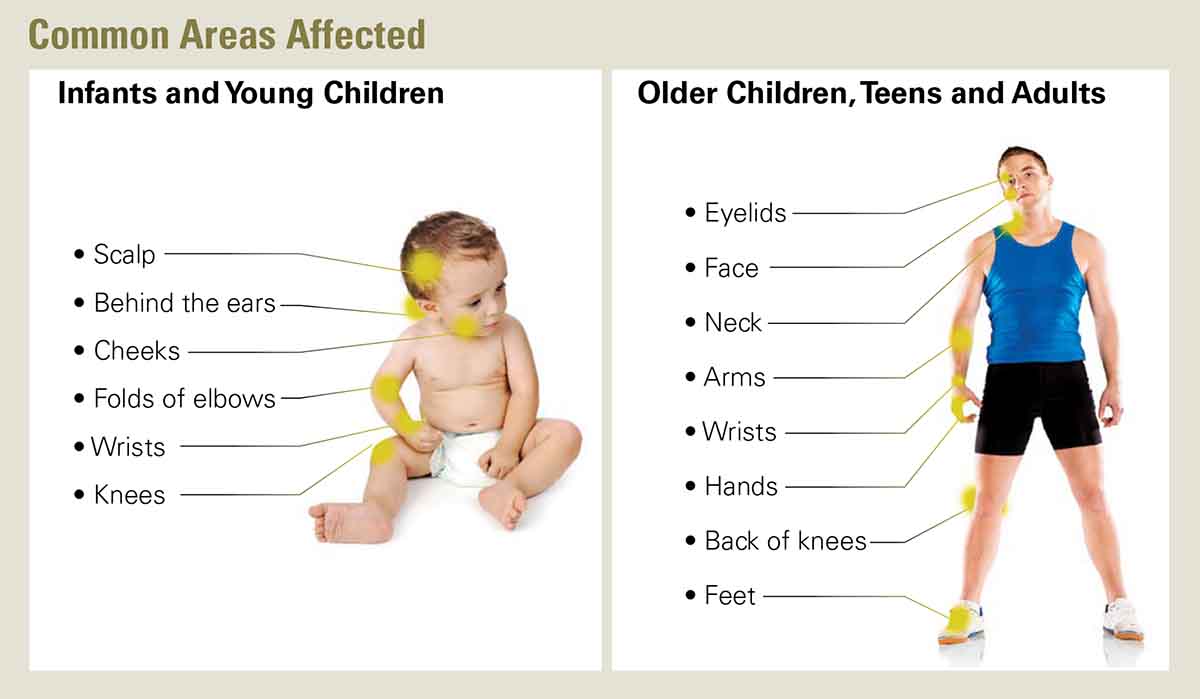
Eczema often appears on the following parts of the body:
- face
- neck
- hands
- wrists
- elbows
- knees
- ankles
- feet
What are the different types of skin changes associated with eczema?
If you were to open a dermatology textbook, you would be flooded with terms used to describe skin conditions and their manifestations. While people with eczema may not need to know all the different terms used to describe eczema, it may be helpful to understand some of the more common ones. These describe the abnormalities, or skin lesions, associated with eczema.
- atrophy – a thinning of the upper layers of skin (or dermis). The thinning makes the skin more fragile and prone to tearing. Atrophy is more common as people age, but it also can be caused by use of topical steroid medications.
- erythema – traditionally described as reddening of the skin. However, in people with darker skin pigmentation, symptoms may be less obvious. There may be areas of darker, ashen gray, or purple skin.
- follicular accentuation – inflammation of the hair follicles. This may present as a rash that looks like goosebumps.
- hyperpigmentation – patches of skin that are darker in color than the surrounding skin.
- hypopigmentation – patches of skin that are lighter in color than the surrounding skin.
- lichenification – thickening of skin patches caused by chronic scratching. Lichenified skin may appear red or darker than surrounding skin.
- striae – commonly referred to as “stretch marks.” These may present as indented streaks or streaks of darker or different colored skin. Striae can also result from the use of topical steroid medications.
- telangiectasia – dilated or broken blood vessels on the surface of the skin.
- xerosis – excessively dry skin. This may cause itching, skin flaking, or cracking.
See Our Free Eczema Webinars

What triggers eczema?
An important part of an eczema treatment plan is preventing exposure to allergens and irritants that set off skin problems. First things first – you must identify what is triggering your eczema symptoms.
Triggers and symptoms of eczema are different for everyone
What makes identifying them so challenging is sometimes a flare-up can occur hours after the initial exposure. Some people may experience symptoms in certain areas of the body or only at certain times of the year.
Trigger avoidance is essential in managing eczema, but it’s important to remember that, since eczema is a systemic condition, it is not a cure. Following are common eczema triggers.
Contact allergies
Eczema is sometimes set off by something a person is in contact with on a regular basis. It could be a piece of jewelry that contains nickel, rubber or chemicals used in cosmetics, disinfectants and skin products.
An allergist can do a patch test to identify the specific allergens causing the problem.
Other potential skin allergens include:
- Antibacterial ointments such as neomycin and bacitracin
- Formaldehyde, which is found in some household cleaning products.
Dry skin
When your skin is dry, it can lead to eczema symptoms. Some people have a genetic condition associated with a skin protein called filaggrin that causes their skin to lose moisture and allow allergens and bacteria to enter the skin more easily.
The best way to prevent an eczema flare is to keep your skin well moisturized. Recent research suggests that moisturizing a baby’s skin from birth may help prevent eczema from developing.

Dust mites
These tiny insects live in mattresses, pillows, upholstered furniture – anywhere they can find moisture along with their favorite food, tiny bits of shed human skin.
Eczema patients may be allergic to dust mites. Allergens from their droppings and dead bodies collect in bedding, furnishings and house dust, then irritate skin, airways and eyes on contact.
When eczema is already flaring, dust mite allergens can worsen the problem. Encase your bed’s pillows and mattress with allergen-proof covers to put a barrier between you and the dust mites. Wash linens weekly and vacuum carpets, floors and furnishings with a HEPA vacuum.
Environmental Allergies
People with eczema may experience symptoms after exposure to certain grass, tree or ragweed pollen and/or indoor or outdoor mold.
It’s best to treat symptoms that arise from environmental allergens with aggressive moisturizing, along with antihistamines and topical corticosteroids if necessary.
Skin prick or blood testing for environmental allergies will help identify specific allergens to avoid.
Some patients may do well with allergen immunotherapy (allergy shots or tablets), in which a patient is given a gradually increasing amount of an allergen to build tolerance and reduce symptoms.
Food Allergies
Food allergens can play a role in the onset of eczema symptoms, particularly for infants and young children. Between 35 and 60 percent of young children with moderate to severe eczema also have food allergies.
It’s believed the breakdown of the skin barrier contributes to an allergic response when a food allergen is consumed.
Among children under the age of 2, eczema is most often related to milk or egg allergy, but it can occur with any food. Other common food allergens include peanut, tree nuts, fish, shellfish, soy and wheat.
Consult with a board-certified allergist for a diagnosis and then develop a plan to avoid the food allergen. Food-allergic patients are also at risk for anaphylaxis, a severe allergic reaction. Always carry two epinephrine auto-injectors, the treatment for anaphylaxis, if you have a severe food allergy.

Pet Allergies
Pet dander (dead skin cells), saliva or urine are normally harmless proteins, but for people with eczema they can trigger skin symptoms leading to respiratory problems. Early exposure to pet dander may contribute to the development of eczema in children who are prone to the condition.
Finding a new home for the furry pet is the most effective way to reduce levels of pet allergens in the home, but if that’s not a consideration, bathe your pet at least once a week and set up no-pet zones, including the bedroom.
Hormones
In women, hormone fluctuations may trigger or worsen eczema symptoms. Hormone changes occur just before and during menstruation, during pregnancy, after pregnancy, or when transitioning to menopause.
Outdoor Temperatures
Whether because it dries out skin or causes sweating, heat is a common eczema trigger. Sweat, in particular, can collect in your armpits or inner part of your elbow, leading to skin irritation.
Meanwhile, in winter months, humidity that provides moisture in the air decreases, resulting in dry skin. In addition, a sudden rise or drop in temperature can trigger an eczema flare.
Strategies to keep comfortable in hot and cold weather include:
Hot Weather
- Wear appropriate clothing: light, breathable clothes in the summer.
- Avoid going outside during peak heat times during the day, usually between 10 a.m. and 3 p.m. If you do go outside, keep a small towel with you to wipe away excess sweat.
- Stay hydrated to moisturize from the inside out.
Cold Weather
- Wear gloves in the winter (since hands are particularly sensitive and often exposed to cold).
- Consider a humidifier to moisturize the indoor air.
Skin Irritants
While they are not true allergens, some soaps, shampoos, detergents, fragrances and wool or synthetic clothing can significantly irritate sensitive skin.
Heavy or tight clothing that rubs against the skin can also cause symptoms. Use gentle, nonirritating products and stick with them.
Natural fiber clothing such as cotton or silk is usually most comfortable. Once an area gets irritated, it can take a long time for it to calm down.
Stress
An increase in stress may either cause an eczema flare or worsen an existing one. Some patients may scratch more often when they’re feeling pressure. Managing stress effectively can reduce flares.
Coping strategies such as meditation or yoga, regular exercise, getting enough sleep, and connecting with family and friends are great ways to take your mind off your worries.
Tobacco Smoke
Cigarette smoke, including secondhand smoke, can irritate skin in addition to the lungs and eyes. Set a no-smoking policy both inside and outside your home; smoking is a major health issue for everyone.
Viral and Bacterial Infections
The common cold can cause an eczema flare. In addition, the herpes virus, which can cause cold sores in and around the mouth, can lead to flares – including a potentially serious infection that can spread cold sores to other areas of the body.
Exposure to bacteria can cause harmful toxins to secrete into the skin, prompting an immune reaction and causing skin inflammation. One of the more common bacteria is Staphylococcus aureus, which can not only worsen eczema but also slow skin healing.

Eczema occurs in all races and ethnicities, but it has a unique appearance in people of color. See our partner website for more information ⤑
How is eczema diagnosed?
Patients can undergo testing to find out what allergens and irritants are worsening their symptoms. Know what triggers your eczema puts you one step closer to reducing symptoms, whether through avoidance, medication or other treatments.
Skin Prick Tests
Droplets of suspected allergens are placed on or just under the skin surface. Raised bumps (about the size of a mosquito bite) strongly indicate an allergy to the substance. Skin prick testing is commonly used by allergists because of its accuracy, ease of use and immediate results. Results are typically known within 20 minutes.
Blood Test
After a blood sample is drawn, it is analyzed to detect IgE antibodies directed at specific allergens. Tests may measure specific or overall levels of IgE Some may also break down common allergens and measure IgE to specific components. Lab results may take several days. Consult with your doctor to ensure that the blood test is interpreted correctly. Eczema typically results in very high IgE levels and may falsely elevate results.
Patch Test
Chambers containing chemicals of potential triggers on adhesive strips are placed on the patient’s back. After 2-3 days, the patches are removed by the doctor and the skin is evaluated for reactions. If symptoms appear, then it’s confirmation of an allergy. Patch testing is commonly used for contact allergies to fragrances, detergents, metal and other chemical substances.
Oral Food Challenge
If it’s believed that a food allergy is causing symptoms, the doctor may want to perform an oral food challenge. In this test, the patient is asked to eat a tiny amount of a suspected allergen, and then gradually larger amounts, to determine if there’s an allergic reaction. The challenge should only be conducted by a doctor and at a medical facility that has access to epinephrine and other emergency treatments.

Other tests helpful in diagnosing eczema
Buccal swabs
Buccal swabs, or cheek swabs, are used to detect mutations in the filaggrin gene, the protein that helps protect the body from allergens and bacteria; a lack of filaggrin weakens the skin barrier, leading to eczema.
Skin biopsy
A skin biopsy, where a tiny piece of skin is removed and analyzed under a microscope, can rule out other skin diseases such as skin cancer or psoriasis.
After testing, your doctor will compile all of the evidence together – test results, your personal and family health history, physical exam, home and work environments, activities that might expose you to allergens – to reach a diagnosis.
What other conditions look similar to eczema?
Another challenge of diagnosing eczema is that there are other skin conditions that may appear to be eczema or have similar symptoms to eczema. As a result, people can experience symptoms and not get the right treatment due to misdiagnosis or delayed diagnosis.
These skin conditions may include
- psoriasis
- scabies
- allergies
- hives
- ringworm
- acne
- cutaneous t-cell lymphoma
- Netherton disease
- hereditary angioedema
- chronic idiopathic urticaria
Many of these conditions may have similar appearances to eczema or even overlap with eczema.
That’s why it is very important to work with an allergist or dermatologist for diagnosis and treatment.

What treatments are used for eczema?
Early diagnosis and treatment are essential to avoid skin complications and improve quality of life.
- moisturizers
- medications
- wet wrap therapy
- phototherapy
How do I cope with the challenges of eczema?
If you have eczema, you know that it can greatly affect your quality of life and well-being. The itching, scratching, loss of sleep and more greatly impact day-to-day living. It can also take an emotional toll on both patient and family. Although there’s no cure, there are now better treatments available that can help manage eczema.
In addition to treatments, managing the itch-scratch cycle is the best thing to do to help cope with eczema and reduce symptoms. Also, be sure to practice good self-care and seek out the support you need and deserve with this difficult condition.
Are there other conditions that may look like eczema but are not eczema?
Hereditary Angioedema
Psoriasis
Chronic Idiopathic Urticaria (CIU)
Cold Urticaria
Eczema Items in Online Store
Eczema Webinars
Eczema Statistics
Reviewed by:
Weily Soong, MD, is a board-certified allergist and immunologist and Chief Medical Officer with Allervie Health (previously Alabama Allergy & Asthma Center). Dr. Soong also serves as Medical Director of the Clinical Research Association of Alabama.
Luz Fonacier, MD is Professor of Medicine at NYU Long Island School of Medicine and is the Head of Allergy and Training Program Director in Allergy and Immunology at NYU Winthrop Hospital. In 2020-21, she served as President of the American College of Allergy, Asthma & Immunology (ACAAI), becoming the fourth woman and first Asian American to serve in that role.
