Managing Asthma in School: A Guide for Parents
- Home
- |
- Allergies and Asthma at School...
- |
- Managing Asthma in School: A...
A healthy school environment is essential for children with asthma. Healthy schools are essential for general well-being as well as academic performance. Asthma is the number one reason for children missing school days. We can create a positive school environment for children with asthma by managing triggers and medications effectively.
It’s important for parents and schools to work as partners to care for students with asthma. Parents should communicate their child’s asthma needs to school staff and provide the necessary medication and paperwork. School staff and school nurses should develop school health policies and plans so they are prepared to deal with asthma at school.
Allergy & Asthma Network has numerous resources to help you keep your child with asthma safe at school.
What can parents do to prepare their child with asthma for school?
Plan ahead and make an appointment with your child’s doctor. Be sure to talk about your child’s asthma, general health and any other concerns you may have. It’s also a good time to update:
- medication permission forms
- prescriptions for medication to leave at school
- school forms and care plans – Asthma Action Plan
- physical form when needed
Make an appointment before the first day of school with the school staff and/or school nurse. At this appointment, you can:
- Share any updates with the school or school nurse about your child’s health.
- Describe any asthma issues from the summer months.
- Discuss asthma triggers and any accommodations needed for your child.
- Provide your child’s school or school nurse with up-to-date forms and asthma medications, such as an Asthma Action plan and any prescribed medications.
- Give the school written permission to discuss your child’s health with your child’s healthcare team.
This is also a good time to provide your child’s school or school nurse with up-to-date forms and medications:
- Quick-relief albuterol inhaler (if prescribed) and any other prescribed medication
- Medication permission from parent and provider
- Asthma Action Plan
COVID-19 Back to School Recommendations

It’s good for parents to know some basic facts about asthma:
- 1 in 10 children are diagnosed with asthma
- 24+ million Americans are diagnosed with asthma
- 13.8 million school days are missed each year due to asthma – #1 reason students miss school
- 3 in 5 people limit their physical activity (should not have to limit activity if asthma is in control)
- Studies show schoolchildren with asthma struggle more in class when their symptoms are not well controlled.
Check in with the school as needed with any concerns about asthma that come up during the school year.
Concerns may include:
- issues in physical education and during recess
- treatment (if needed) during field trips
- understanding of asthma by school staff and readiness to treat an
- asthma flare
- use of inhaler at home or school
- general questions about asthma medication
- asthma flares at certain times of the year
- asthma triggers
Get a Free Copy of Our "Understanding Asthma" Guide ➤

How can parents handle a change in their child’s condition during the school year?
Be sure to promptly notify the school if your child has a severe asthma attack. Also, communicate changes to your child’s care or any change in your child’s asthma symptoms.
Note the expiration dates of medications that you keep at school or your child carries to school. Replace any expired medication as soon as possible. A good strategy is to put a notice on your calendar for 2-3 weeks before medication expires. This will give you time to get new medication from the pharmacy and deliver it to school.
What should parents do at the end of the school year?
It’s a good idea to continue communication with the school or school nurse as each school year comes to a close. You should:
- Take time to talk with your child about the school year and how to prepare for continued success at school.
- Set aside time to pick up any medication brought to school.
- Ask the school for any healthcare or medication forms needed for the next school year.

There are so many different inhalers or other tools with asthma – how can I better understand these?
Asthma care is constantly evolving, and new medications are available to address common asthma triggers. It’s important to help keep your child’s asthma in control. Talk to your healthcare provider to determine the best course of action and determine if it’s time to see an asthma specialist. It’s understandable that it’s overwhelming. Here is some helpful information to manage asthma.
Resources from Allergy & Asthma Network include:
- Asthma medications and treatments
- Respiratory Treatments Poster with up-to-date resource with all inhalers and treatments available
- Respiratory Tools Poster includes: holding chambers / spacers and nebulizers (scroll below Respiratory Treatments Poster)

How do I know when to keep my child home from school?
It can be hard to know when a child with a chronic disease like asthma should go to school and when to stay home. The COVID-19 pandemic has made those decisions even harder. Use your child’s personalized Asthma Action Plan as a guide. It will identify symptoms to watch for and treatments to follow at school.
Good communication among parents, teachers and students is essential. Notify the school nurse and teachers if your child is in pre- or post-asthma flare stages but controlled with medications.
Missing school can also cause anxiety in some children. Keep in mind that anxiety symptoms can sometimes mimic asthma. If you think your child is not feeling well due to anxiety, call your healthcare provider to get help for your child.
This resource can help you to make a sound decision related to your child’s symptoms.
| When to Go to School | When to Stay Home |
|---|---|
| No fever for 24 hours | Fever of 100.4° or higher |
| Has energy to participate in school activities | Feels too sick to participate in school activities |
| Occasional cough | Moderate to severe cough |
| Feels good | Shortness of breath |
| No vomiting or diarrhea for 24 hours | Stomach pain |
| Sore throat | |
| Vomiting | |
| Diarrhea | |
| Neck pain | |
| Rash | |
| Bloodshot eyes | |
| Feels extra tired | |
| Needs fever or pain medication to feel good |
For Students with Asthma
| When to Go to School | When to Stay Home |
|---|---|
| Slight wheeze | Sleepness night due to asthma symptoms |
| In Green Zone on Asthma Action Plan | Significant wheezing, coughing, shortness of breath |
| Experiencing asthma flare that is not well controlled with quick relief medication |
What asthma symptoms should my child immediately bring to the attention of the teacher?
It’s important for school staff and classroom teachers to be able to identify asthma symptoms, including the signs of an asthma attack. Symptoms may include:
- Wheezing – a scratchy or whistling sound from lungs when breathing
- Shortness of breath or rapid breathing – possibly associated with activity
- Chest tightness or pain
- Fatigue – student may stop playing or avoid activity
- Coughing – may be continual or happen often
When should my child see a specialist for their asthma?
It may be time to have your child see an asthma specialist if:
- Your child is having numerous attacks throughout the year
- Your child is having asthma flares that aren’t controlled by the treatment your doctor has prescribed
How can parents work together with teachers and school nurses to reduce the risk of asthma flares in the classroom?
Talk with your child’s teachers and the school nurse about asthma triggers that may be in the classroom. Some common classroom triggers include:
- Mold from excess moisture in the building
- Cockroaches, mice and other pests
- Dander from animals in the classroom
- Dander brought in on clothing from pets at home
- Secondhand smoke
- Chemicals from cleaning products
- Perfume, cologne and/or plug-in air fresheners
In addition, outdoor allergens and irritants such as pollen or school bus exhaust can enter classrooms through open doors or windows.
Work with the teachers, school nurse and custodial staff to remove potential triggers such as mold. It could be as simple as closing windows and doors to keep pollen and school bus exhaust out of the classroom.
Find out what cleaning products the custodians use and whether it could trigger an asthma attack. Ask that teachers don’t keep a furry classroom pet, don’t wear perfume or cologne, and don’t use plug-in air fresheners.
What types of care plans are there at school?
There are four main types of care plans at school:
- Individualized Healthcare Plan (IHP): this plan is written in nursing language for nurses to direct complex nursing care. This document should be updated regularly and outline planning, nursing interventions & treatments, education and emergency response.
- Emergency Action or Care Plan (EAP or ECP): this plan is written in easy-to-understand language for all school staff and outlines the steps to take in the event of a medical emergency
- Section 504 Plan: This is a legally binding plan written in educational language. It ensures accommodations for a student with a chronic health issue.
- Individualized Education Plan (IEP): this plan is a written statement of special education needs – only used in asthma if an educational disability exists

Asthma and sports in school
As long as your student’s asthma is under control, exercise offers many health benefits.
- Improves heart health
- Boosts mental health – improves mood, reduces feelings of depression, improves overall well-being, empowers the student to feel more in control
- Reduces risks of many health concerns – helps with weight control, good for muscles & bones, promotes skin health, boosts energy, promotes better sleep
Tips for exercise or sports:
- Check with your doctor before beginning any exercise.
- Build up endurance sensibly.
- Avoid exercising in cold, dry environments.
- Pay attention to your body as you exercise.
- Pre-medicate with an inhaler if needed or recommended by your child’s doctor.
How can parents work together with athletic coaches and gym teachers to help student-athletes manage their asthma?
Parents, physical education teachers and athletic coaches should meet at the beginning of the school year to discuss a child’s asthma. They can also meet prior to the start of a sports season.
Parents should provide an updated Asthma Action Plan to coaches. This should include a list of symptoms to watch for that indicate an asthma attack. Ask coaches to keep the Asthma Action Plan with them, such as on their clipboard during practices or games.
Make sure your child always has a quick-relief albuterol inhaler at gym class, practice and games. The child, the gym teacher and coach should know where the quick-relief inhaler is at all times. If the school has stock albuterol, the coach and gym teacher should have quick and easy access to the medication in an emergency. They should know how to administer the medication in an emergency.
Parents should stay in touch with the coach throughout the sports season and keep them aware of any changes to the child’s condition or treatment plan.
What is the September Asthma Peak?
Approximately 25% of all children’s asthma hospitalizations occur in September. Doctors even identified the third week of September as the peak week for hospitalizations and ER visits.
What can you do?
Read: 10 Ways to Stay Healthy During the September Asthma Peak Week
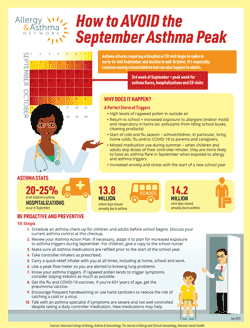
Download a FREE Copy of How to Avoid the September Asthma Peak
What is the school’s responsibility to reduce asthma triggers at school?
It’s important for your child’s school to create an asthma-friendly environment through policies and practice. Schools should be aware of students’ environmental asthma triggers and work to reduce exposures to those triggers.
Schools should be aware of indoor air quality as well as daily outdoor air quality information. Accommodations, including limiting outdoor activity, can be made on days that have an unhealthy air quality index level. Allergy & Asthma Network has an Asthma, Allergy and Flu Index that can be helpful.
It’s important for schools to be aware that cleaning products can trigger asthma due to its odor and chemical contents. Be aware of what the school uses to clean floors and surfaces.

Questions & Answers on Asthma at School (Q&A)
The following is a list of questions we often get from schools, parents, and school nurses.
What are the most common triggers for asthma attacks in school?
The Environmental Protection Agency identifies the most common asthma triggers at school as:
- cockroaches and other pests
- mold resulting from excess moisture in the building
- dander from animals in the classroom
- dander brought in on clothing from animals at home
What can schools do to reduce the incidence of asthma attacks?
Schools can assess indoor air quality as a part of their program to reduce triggers for asthma in school. Knowing students’ triggers and removing as many as possible from the school environment can improve breathing and possibly reduce the need for medication.
Does school bus exhaust trigger asthma?
School bus exhaust releases small particles into the air that can settle deep into student’s lungs. The particles can contain toxic air pollutants that can irritate the airway and cause or worsen asthma symptoms.
Should my child with asthma go to school during the COVID-19 pandemic?
Yes, your child with asthma can attend in-person school during the COVID-19 pandemic. It’s important that your child’s asthma is well controlled before going to school. This includes:
- taking asthma medications as directed;
- knowing potential asthma triggers at school and avoiding them;
- following the Asthma Action Plan.
If your child’s asthma is not well controlled, then it may be best for the child to stay home. Children with moderate to severe asthma may be at higher risk for getting very sick with COVID-19.
Discuss any concerns with your child’s pediatrician or asthma specialist. Speak with the school nurse and/or teachers. It’s best to do this prior to the school year. CDC recommends that your child get both the annual flu shot and COVID-19 vaccine.
If your family lives in a community with high levels of COVID-19, then it’s recommended that your child wear a face mask at school. Check with your school and local or county health department to confirm.
How does asthma affect school attendance?
What is an asthma care plan?
There are several kinds of care plans used for asthma at school:
- Asthma Action Plan – outlines asthma care based on symptoms
- Individualized Healthcare Plan – for students that require more complex care at school. It’s written by the school nurse to direct nursing care.
- Emergency Care Plan – for students whose asthma is likely to result in a medical emergency. It’s written in non-medical language to help guide school staff.
Who can fill out an Asthma Action Plan?
What should be included in an Asthma Action Plan?
Asthma Action Plans usually provide the child and family with steps to follow depending on their current symptoms:
- Green Zone – Daily care when symptoms are under control
- Yellow Zone – Actions to take when student is beginning to experience an asthma attack
- Red Zone – Steps to follow when asthma becomes an emergency
How do you complete an Asthma Action Plan?
Are the Asthma Action Plan, Asthma Individualized Healthcare Plan and Emergency Care Plan all the same thing?
The Asthma Action Plan is created by your child’s doctor or healthcare provider and directs care on a daily basis as well as when asthma symptoms get worse.
The Asthma Individualized Healthcare Plan (IHP) is a nursing document written in nursing language that includes asthma care, equipment needed, educational needs and classroom accommodations needed for the student to attend school.
The Emergency Care Plan (ECP) is often not used if an Asthma Action Plan is in place. The ECP outlines the steps to take in an emergency and is written to be followed by school personnel.
Are inhalers allowed in schools?
Can children with asthma participate in sports?
Reviewed by:
Eileen Censullo, RRT, is a respiratory therapist. She currently serves as Director of Network Relations for the American Heart Association. She was on the executive board of the Pennsylvania Society for Respiratory Care from 1995 to 2015. She has also served as Respiratory Care Manager at Taylor Hospital in Ridley Park, Pennsylvania.
