Skip to 10 Ways to Stay Healthy
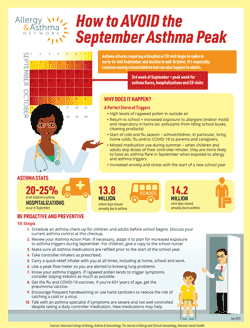
Are you or a loved one among the 25+ million people in the United States living with asthma? If so, it is important that you are aware that September is a peak time for asthma attacks. It’s called the September Asthma Peak. This is when emergency department and hospital admissions for asthma tend to increase, especially among children.
As September unfolds, the spike continues to rise. The September Asthma Peak Week is the third week of the month, when asthma-related ER and hospital visits spike to their highest level. Physician visits for asthma also tend to spike in September and early October.
Why does this happen? September is a time when adults and children are exposed to more allergy and asthma triggers such as ragweed pollen, indoor and outdoor mold and respiratory viruses. It’s especially problematic for children exposed to more asthma triggers after school starts in September. These triggers can cause asthma attacks.
How common is Asthma Peak Week?
Asthma epidemics in the month of September have been reported in many countries, mostly in the Northern Hemisphere. These countries include the United States, Canada, the United Kingdom, Mexico, Israel, Finland and Trinidad. It’s estimated that between 20% to 25% of all childhood asthma attacks requiring hospitalization occur during the month of September.
The September Asthma Peak phenomenon first made headlines in the early 2000s. Cases of September asthma flare-ups were at their highest in 2005. Since then, cases have declined slightly and stabilized. September remains the leading month for asthma attacks requiring hospitalizations.
Why does the September Asthma Peak happen?
The rise in asthma episodes in September is caused by a perfect storm of circumstances:
- Exposure to viruses such as the common cold, the flu, COVID-19, and other respiratory infections. Studies cite respiratory viruses as the primary trigger for asthma attacks in September.
- Returning to school increases exposure to indoor allergens. These include dust mites, mold and pet dander. Exposure to lung irritants – such as air pollutants from idling school buses – also increases. The same thing can happen at work and office buildings with idling cars in parking lots or garages.
- Breathing in high levels of ragweed and mold allergens.
- Stopping or forgetting to take your daily controller inhaler during the summer. This can cause underlying inflammation in the lungs and impact disease control. It puts you at risk for asthma flares in September when you’re exposed to more allergens and irritants.
- Anxiety about the new school year or increased stress levels at work following the summer.
Keep in mind that while the spike in asthma flare-ups is highest during the third week of September, asthma flares can happen anytime. In some areas of the United States, the September surge in cases can begin in late August and continue through mid-October.
What are common asthma symptoms?
The most common asthma symptoms are coughing, wheezing, chest tightness and shortness of breath.
Coughing from asthma is often worse at night. This is called nocturnal asthma and can lead to disrupted sleep. If asthma wakes you up more than twice a month, this is a sign of uncontrolled asthma.
Some other symptoms may include fatigue or a general feeling of low energy, difficulty sleeping and increased mucus production. A bluish tint to the skin and fingernails is a sign of an asthma attack.
What are some common triggers of asthma in September?
September is a month of transitions. It’s the end of summer and the start of fall. The heat and humidity may decrease but ragweed is in full bloom.
September is also the time when the weather starts to turn cooler and people spend more time indoors. The U.S. Environmental Protection Agency (EPA) estimates that people spend 90% of their time indoors. That means children and adults are sharing germs during cold and flu season and they are exposed to more indoor allergens.
Common asthma triggers:
- Viral respiratory infections. Any respiratory infection can be more severe for people with asthma. A cold, the flu, and COVID-19 are all highly contagious, These viruses can cause ER visits and hospitalizations.
- Indoor allergens. More time is spent indoors at school, work, or other indoor activities. This increases exposure to asthma and allergy triggers. Common indoor triggers include mold, pet dander, dust mites, cockroaches and mice. Any of these can cause allergies to flare up, and trigger an asthma attack.
- Outdoor allergens. Ragweed pollen is a strong allergen that blooms in early August and sticks around until first frost. Outdoor mold counts can also trigger symptoms. Raking or picking up damp leaves in the fall can expose you to mold.
- Irritants. Diesel exhaust from idling school buses and city buses can linger in the air. Fumes can also enter classrooms and offices through open windows and vents.
- Tobacco smoke and vaping. Cigarettes and vapor from e-cigarettes are asthma triggers. People with asthma who also smoke are at risk for asthma flares. Inhaling smoke or e-cigarette vapor secondhand can also cause an asthma flare. Thirdhand smoke (smoke that clings to clothing, furniture, etc.) is increasingly a problem for people with asthma as well.
- Exercise-induced asthma. Physical activity or participating in sports in September can trigger symptoms, especially when outdoors while ragweed pollen is at its peak.
- Stress. School, work, and social activities can cause stress and lead to an asthma flare.
- Cold air. In some parts of the United States, cold air arrives in September. People with asthma can have an asthma flare due to cold air or sudden changes in temperature.
- Strong smells. Strong smells such as perfume, cologne or hair products can cause asthma symptoms. Some offices and school classrooms sometimes use essential oils, scented candles or air fresheners that can trigger asthma. Cleaning products can also have chemicals and strong odors.
Download a FREE Copy of How to Avoid the September Asthma Peak
Does September Asthma Peak Week affect adults differently?
Most September asthma research focuses on the impact on children, but it’s clear that adults are affected as well.
Adults with asthma are at risk of emergency department visits, hospitalizations and deaths. They are at greater risk of severe symptoms or dying from an asthma flare than children. The highest annual rates of death from asthma, according to CDC, is the 35-65 age group followed by the 65+ age group. People in those age groups are eight times more likely to die from asthma than children.
Respiratory viruses including the flu are one of the primary causes of asthma attacks in the fall. Adults with children may be at risk of increased exposure to viruses and germs. When children return to school in August and September, they tend to share viruses and germs amongst each other. Then they bring those viruses and germs home to their family. Before you know it, everyone in the whole house is sick.
Respiratory viruses can lead to asthma flare-ups. Older adults with asthma, in particular, can become very sick from respiratory illnesses as they tend to have weaker immune systems.
What are 10 ways to stay healthy during the September Asthma Peak?
Preparation is the key to staying healthy during the September Asthma Peak. Here are 10 things you should plan for in the days leading up to and during the month of September:
- Schedule an asthma checkup for all family members before September. Discuss your current asthma control at this checkup. Uncontrolled asthma will increase your risk of flare-ups heading into the fall.
- Review your Asthma Action Plan. This is a treatment plan you develop with your doctor that details what you should do if you develop asthma symptoms. If necessary, adapt the Asthma Action Plan if your exposure to asthma triggers is higher during the month of September. Update your child’s Asthma Action Plan and make sure the school nurse has a copy.
- Make sure all asthma medications are refilled leading up to the month of September – including before children return to school. Double check the expiration date on your quick-relief inhaler.
- Take controller inhalers as prescribed, including during the summer months. Studies show the lowest fill rate for asthma medications is in July. At doctor appointments, show how you use your inhaler to confirm you are using it correctly.
- Keep or carry medications at school and work, especially a quick-relief inhaler to treat sudden asthma attacks.
- Use a peak flow meter. This is a device that can signal brewing lung problems and alert you to a coming asthma attack.
- Identify and avoid asthma triggers, especially if you or your child has allergic asthma. If ragweed season is a problem, exercise indoors. For schoolchildren, talk with teachers about offering the option of staying inside during recess or gym class. Ask if the school can keep windows closed and keep pets out of classroom to avoid animal dander. Talk with the custodial staff to find out what cleaning chemicals are used in school buildings. It may be worth it to take these extra precautions.
- Get the flu and COVID-19 vaccines early to prevent infections and/or severe symptoms. Flu vaccines are usually available at pharmacies by late August.
- Encourage frequent handwashing to reduce the risk of catching a cold or a virus. Many schools and workplaces are providing hand sanitizers.
- If you have severe asthma that is not well controlled despite taking a daily controller medication, talk with an asthma specialist. It’s important to have good asthma control at all times of the year. New precision medications called biologics are available. These medications target the source of symptoms at the cell level rather than treat the symptoms themselves.
What are some ways to get involved in self-managing asthma to avoid flares?
It’s critical that people with asthma continue taking their daily controller inhaler as prescribed to prevent inflammation. Controlling inflammation will help reduce the likelihood of an asthma flare once a trigger is encountered in the fall.
Identify and reduce your asthma triggers and know when and how to use your inhalers. Work together with your doctor to determine what triggers your asthma. It may be helpful to take notes of what potential allergens and irritants you were exposed to prior to symptoms.
Doctors and pharmacists can review your inhaler technique with you to make sure you are getting the most medicine out of your inhaler. Ask your doctor about using a valved holding chamber or spacer. These are handheld devices that attach to the inhaler and trap the medicine so it goes directly into your lungs. They are especially helpful for children and older adults who may not have the ability to coordinate breath and activate a metered-dose inhaler.
It’s also important to make sure you have a strong immune system to fend off respiratory viruses that begin to increase in September.
What are some tips to boost your immune system?
Healthy lifestyle choices and basic hygiene can help boost your immune system or your child’s immune system. This can help prevent the spread of germs at home, school and work year-round. It’s also an important part of reducing the risk of an asthma attack.
Make sure all family members get the flu And COVID-19 vaccines before school starts.
The flu vaccine is recommended for everyone ages 6 months and older. It’s especially important for children, people with chronic diseases such as asthma, and older adults. The COVID-19 vaccine is also recommended to help fend off the coronavirus and reduce the risk of severe illness.
Reduce daily stress.
Stress can impact our ability to fight illness. Develop daily routines to make your day less stressful. Practicing yoga or meditation and listening to music can help. Talk with a close friend to help relieve stress.
Exercise every day.
Regular, moderate exercise can keep your lungs healthy. This can include 30 minutes of exercise five times a week for adults, and 60 minutes of exercise every day for children. Daily physical activity also helps heart health and leads to a greater sense of well-being.
Eat a healthy diet.
Eat a balanced diet high in fruits, vegetables and whole grains and low in saturated fats. This can contribute to good health and support a healthy immune system. It’s also important to stay hydrated, especially if it’s warm outside. Keep a bottle of water close by during the day.
Get enough sleep.
People who don’t get enough sleep have less ability to fend off colds, flu and other illnesses. Sleep needs vary for each person and by age, but on average adults need 7-9 hours of sleep a night, and school-age children need 9-11 hours of sleep.
Establish good personal hygiene.
Wash hands often and cover your cough/sneezes with your elbow. These simple actions keep germs from spreading and can protect you and those around you.
Reviewed by:
JACQUELINE EGHRARI-SABET, MD is board-certified in allergy, immunology and pediatrics. She is the Medical Director of Telehealth for Allergy & Asthma Network. Dr. Eghrari-Sabet is the founder of Family Allergy & Asthma Care and the FAAR Institute in the Washington, DC area, where she has been in private practice since 1994. Dr. Eghrari-Sabet is Assistant Clinical Professor at George Washington University School of Medicine and Health Sciences where she mentors the next generation of doctors. She is also President of White Coat Resources, a health education consulting service.

 810304 Eaton Place, Suite 100
810304 Eaton Place, Suite 100