Hives on Black Skin and Other Skin of Color
Hives, also known as urticaria, can happen on any skin tone. The cause is the same for everyone. But hives may look different on darker skin. This can make them harder to notice or diagnose. Some healthcare professionals may even confuse them with other skin conditions like eczema or dry skin. That’s why it’s important to understand how hives show up and feel on Black skin and other melanin-rich skin.
Hives are not a rash, and they are not contagious. Hives are raised, itchy bumps on areas of the skin. When they last more than 6 weeks, it’s called chronic hives (or chronic urticaria).

What causes hives on Black skin?
There are many reasons a person might get hives. Some hives are caused by something easy to figure out, like an allergy. But sometimes, hives show up without a clear reason and keep coming back for a long time.
Doctors group hives into two main types:
- Hives with a known cause, like an allergy, infection, or physical trigger
- Hives with no known cause, which may be linked to the immune system
Hives with a known trigger
Some hives are triggered by touch, heat, cold, or even sunlight. This is called chronic inducible urticaria (CINDU). It means you get hives when you encounter specific triggers.
This group of hives is also called physical urticaria, and includes:
- Dermatographic urticaria: also called “skin writing”
- Pressure urticaria: from tight clothing or items pressing on the body
- Vibration urticaria: from activities like mowing or riding in a car
- Aquagenic urticaria: from contact with water
- Cholinergic urticaria: from exercise or sweating
- Cold urticaria: from being exposed to the cold
- Heat urticaria: from warm weather or hot baths
- Solar urticaria: from sun exposure
Allergic reactions and other triggers
Hives can also happen after eating certain foods, taking medication, or getting a bug bite. They may show up during a viral illness or after a stressful event. These hives usually go away quickly and are not considered chronic.
Hives without a clear cause
Sometimes hives appear with no clear trigger. This is called chronic spontaneous urticaria (CSU). It means the hives come on their own and last for more than 6 weeks.
In some people, CSU is linked to the immune system. Instead of protecting the body, the immune system becomes confused and attacks healthy cells. This is called an autoimmune reaction. People with CSU may also have other autoimmune conditions, like thyroid disease or lupus.

Symptoms of chronic hives on skin of color
Chronic hives are itchy, raised welts that come and go. They can show up in different places on the body and often appear without warning. Hives are considered chronic when they last longer than 6 weeks.
Hives may not always be easily visible on darker skin, but that doesn’t make the symptoms any less real or intense. In some cases, itching or discomfort may happen before any hives appear or even without any at all.
Here’s what to look for:
- Itching that feels deep or constant, even before hives appear
- Itching or discomfort with no visible hives
- Burning or tingling in the skin
- Raised welts or bumps that may be skin-colored, brown, purple, or gray
- Angioedema (swelling) around the lips, eyes, hands, feet, or genitals
- Symptoms that come and go, often without a clear cause
Symptoms are often worse at night or when triggered by heat, pressure, or stress. They may keep coming back. This can affect your sleep, daily life and mental health – especially when others can’t see what you’re going through.
Because chronic hives may look different on Black or Brown skin, they can be missed or misdiagnosed. That’s why it’s important to speak up about how you feel, even if your skin doesn’t “look” irritated.

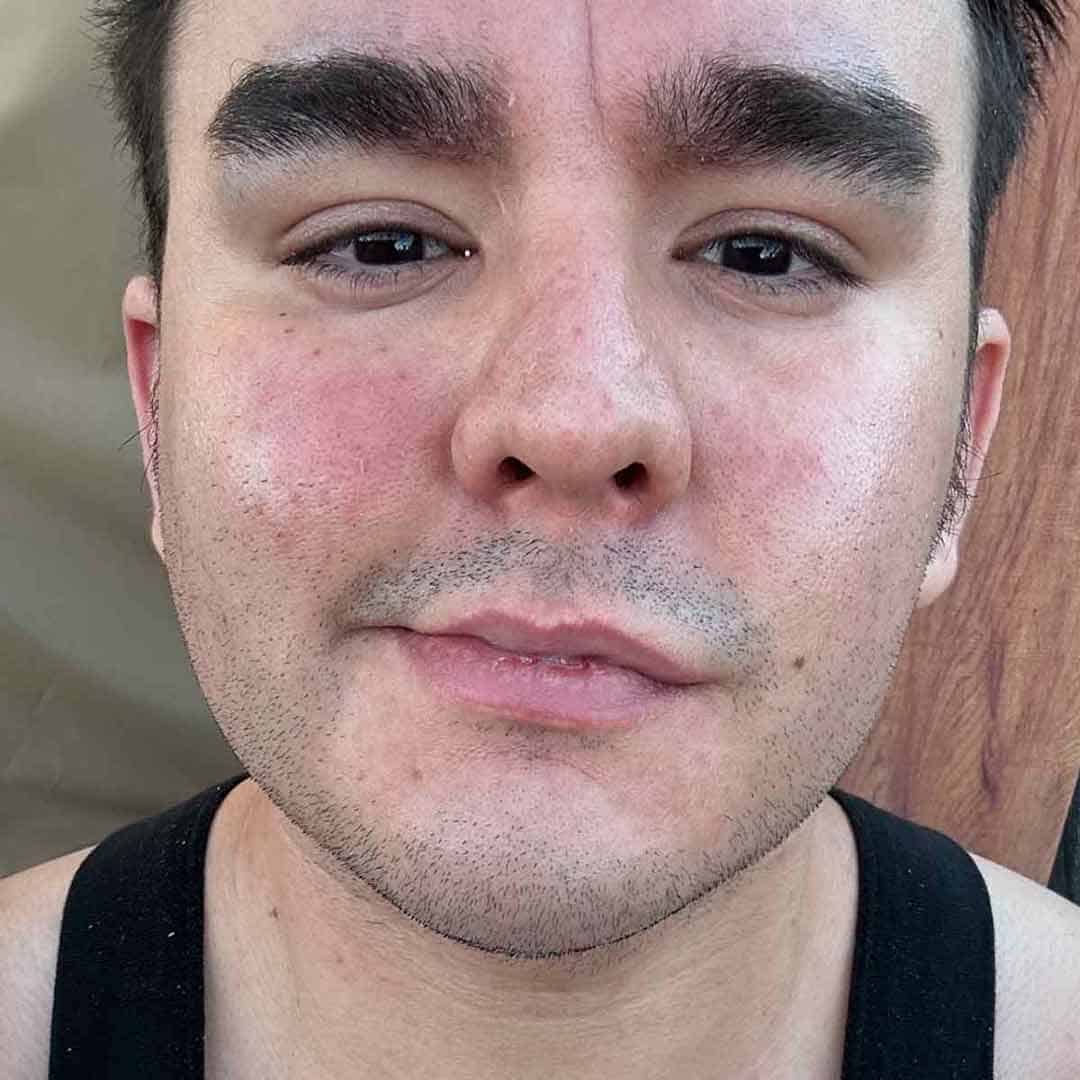
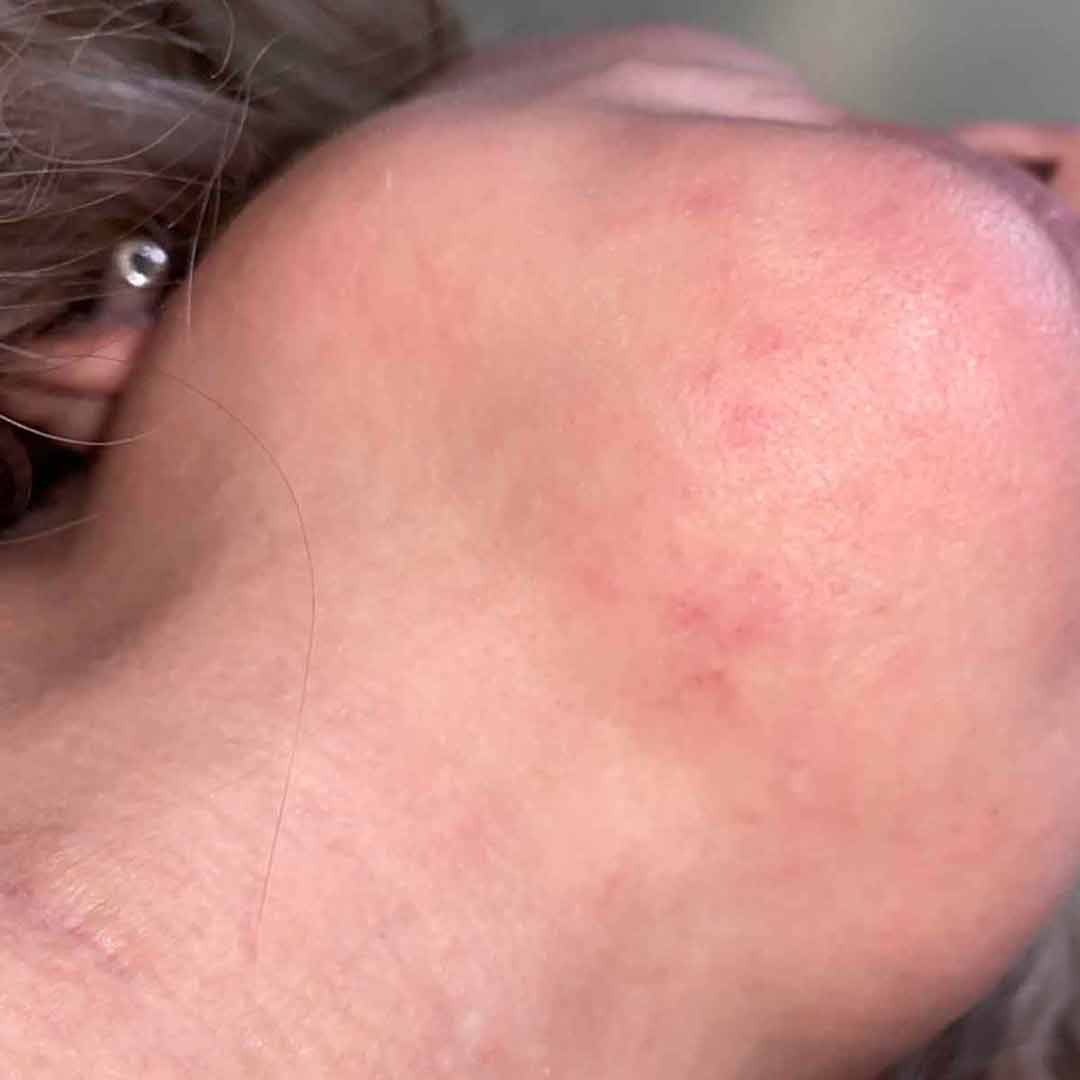
What do chronic hives look like on skin of color?
Hives on Black and Brown skin don’t always look like the pictures shown in textbooks or online. Most medical images show hives on light skin, where they appear red or pink. But on darker skin tones, hives can look very different.
Hives on melanin-rich skin may appear:
- The same color as your skin
- Darker than your skin tone
- Gray or purplish
These differences can make hives harder to see, especially in certain lighting. Because they don’t look the way many healthcare professionals were trained to recognize, hives on darker skin are sometimes missed or mistaken for something else.
In addition to the color of the hives, there are other reasons why hives on darker skin may not be easily recognized, diagnosed or treated quickly.
Hives on dark skin do not blanch
In determining if the welts are hives, doctors often check if hives are blanchable. This means the hives turn white when pressed. But on skin of color, blanching may not be visible. This can lead to missed or delayed diagnoses.
Dermatographism looks different
Some people also develop dermatographism, also called “skin writing.” When the skin is scratched or rubbed, it forms raised lines. Again, this may look a different color than red or pink on darker skin.
- On light skin, the lines look red or pink.
- On darker skin, they may appear dark brown, purple, or gray and may not be as easy to spot.
Hyperpigmentation occurs
After hives fade and heal, some people with skin of color are left with dark spots. This is called hyperpigmentation, and it can last for weeks or even months.
The emotional impact of hives is not taken seriously
Hives that are hard to see may be dismissed or misunderstood, even by healthcare professionals. This can delay treatment and make people feel like their symptoms aren’t being taken seriously.
Living with visible or hard-to-explain skin changes can be frustrating. It can affect your confidence, relationships and mental health. That’s why it’s important to describe what you feel, even if others can’t see it.

How are hives on skin of color treated?
Treatment for chronic hives is the same for all skin tones. Doctors may recommend:
- Daily antihistamines to help with itching and swelling
- Topical corticosteroids or itch creams
- H2 blockers that stop the release of histamine
- Oral corticosteroids or leukotriene modifiers for severe flare-ups
- Biologics (injections) for more serious or long-term cases
- BTK inhibitors that block or slow the release of histamine in people with chronic spontaneous urticaria
- Cyclosporine, an immunosuppressive, for when symptoms do not respond to other medicines
Learn more about available chronic urticaria treatments.

Hives on Black skin: quick facts
Patient Stories on chronic urticaria
Living with Solar Urticaria in Sun City: Angel’s Story
Finding Beauty Beyond the Hives: Emmeka’s Story
Building a Supportive Care Team for Chronic Urticaria: Rachell’s Story
Below are photos of chronic urticaria shared with AAN by patients with the condition.
Key Takeaways from Patient-Reported Difficulties of Living with CSU
The CSU treatment disparities research includes an ethnographic study that examined the perception of how people of color (POC) in the United States are treated when they have Chronic Spontaneous Urticaria (CSU). It explored why many do not get recommendations for stronger medications. Researchers interviewed patients to learn about their experiences getting diagnosed with and treated for CSU. They conducted the interviews in Los Angeles and New York City in March 2024.
Here are the main points from the research:
Slides of the main takeaways from: Experiences of People Of Color (POC) In The Diagnosis And Treatment Of Chronic Spontaneous Urticaria (CSU) In Los Angeles (LA) And New York City (NYC), Gardner, Donna et al., Journal of Allergy and Clinical Immunology, Volume 155, Issue 2, AB217
Questions & answers (Q&A) about hives in skin of color
Here are some of the most common questions we are asked about hives. All answers are reviewed by healthcare professionals trained in treating hives. If you have an additional question you’d like to see answered here email our editor.
Reviewed by:
Dr. Nicole Negbenebor is an Assistant Professor in Mohs Surgery and Cutaneous Oncology and Director of the Skin of Color Clinic, Director of Resident Surgery Education, and Director of the HS clinic at University of Iowa Hospitals & Clinics in Iowa City, IA. She completed her Mohs fellowship in the Department of Dermatology at the University of Iowa and attended Yale University for undergrad.
Supported by: