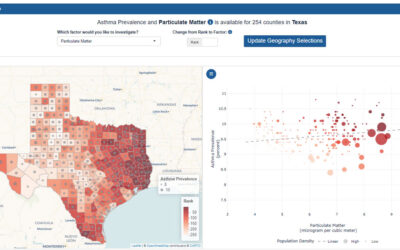
Discover how current asthma prevalence on national, state and local levels can lead to disparities...
Health Disparities
Allergy & Asthma Network Applauds National Academies’ Report to Improve Health Equity
The National Academies of Science, Engineering, and Medicine recommends the federal government integrate health equity in its programs, policies and legislation.
Allergy & Asthma Network Urges Biden, Congress to Prioritize Values-Based Healthcare
Health groups are urging President Biden, Congress to put healthcare, health inequities and lower drug prices at the center of economic recovery.
Asthma, Covid-19, Questions We Need Answered: Black People Like Me Virtual Conference Series
Join us for a free virtual event to better understand and address the impact of asthma and COVID-19 in the Black community.
COVID-19 Vaccine – Treatment, Trust & Health Inequities
In this recorded webinar, speakers give us a COVID-19 vaccine update including challenges in vaccination related to trust and health inequities.
Allergy & Asthma Network Announces National Trusted Messengers Project to Address Health Inequities
The Trusted Messengers project will address inequities in health exposed by the COVID-19 pandemic and improve long-term health outcomes in communities of color.
Allergy & Asthma Network to Host COVID-19, Asthma and COPD Screenings at Atlanta Churches
September 2020 – Allergy & Asthma Network Will Promote Health Equity by Hosting Free COVID-19, Asthma & COPD Screenings at Atlanta Churches.
Disparities in Food Allergy – Racial, Ethnic & Socioeconomic Considerations
Join us on Sept. 24 when Dr. Ruchi Gupta will discuss racial/ethnic differences in food allergy prevalence, outcomes, care and management.
A Tale of Two Asthma Patients: How Social and Economic Factors Impact Asthma
Learn through the stories of two young men with asthma how social and economic factors influence health and access to medical care.
Allergy & Asthma Network Secures PCORI Engagement Award, CDC Grant to Reduce COVID-19 and Asthma Disparities
Allergy & Asthma Network is working to address COVID-19 and asthma health disparities through a PCORI Engagement Award and CDC Grant.
‘Not One More Life’ Makes an Impact on Asthma Disparities in Communities of Color
Learn about Not One More Life, a program of the Allergy & Asthma Network that brings asthma screenings and education to vulnerable populations in the U.S.
Black Individuals at Higher Risk for Contracting COVID-19 – New Research
Learn more about a new study showing that Black individuals were twice as likely as White individuals to test positive for COVID-19.
All About
Asthma and allergies occur in all racial, ethnic and socioeconomic groups, but they are more common in African American, Hispanic/Latino and Native American communities, particularly those living in poor urban areas. Health insurance coverage, income levels, and even where people live contribute to disparities in care. Living in a city with high pollution levels, living in an older building with vermin infesting the home, relying on public transportation, and living with mold can contribute to poor management of asthma and disproportionately affect people along racial and ethnic lines. People of color have higher rates of death from asthma and severe allergies, as well as a higher incidence of emergency department visits and hospital stays.
Allergy & Asthma Network is committed to creating and expanding programs to address the imbalance of care for these populations. The Network provides medication assistance programs and bilingual resource guides and addresses health disparities at the federal, state and local level. Advocacy takes many forms, but affordable access to medication, accessible telehealth solutions for those unable to physically see a doctor, accountability from health insurance and pharmaceutical companies, availability of life-saving medications in schools and public places and reduced pollution of air and water are some of the Network’s key legislative issues.
Some important help the Network recently received was a CDC grant and a Patient-Centered Outcomes Research Institute (PCORI) Engagement Award. The CDC grant will be used to implement national standard-of-care guidelines for asthma patients aimed at reducing ER visits and hospitalizations. The PCORI engagement award will be used for a virtual symposiums that bring together African American patients, as well as doctors, researchers and faith-based leaders to present research and to discuss the opportunities, gaps and barriers in engaging African American patients in patient-centered research.
The Network also reaches out to at-risk people and underserved communities through its Not One More Life Trusted Messengers program, a joint public-private partnership and large-scare community project that offers free COVID-19 testing, asthma and COPD screenings and patient education.
The current COVID-19 crisis has highlight health disparities, finding that African Americans and Hispanic/Latino populations and Native Americans face significantly higher rates of COVID-19 cases, hospitalizations and deaths. Ongoing disparities in physical health and social determinants of health play a role in the number of cases and deaths. Poverty is a significant issue for many racial and ethnic minorities, so some protective measures against COVID-19 may be less feasible. Many may rely on public transportation, have limited access to healthcare, live in close living quarters and may also work in essential jobs, which may increase risk of exposure to the virus.
All of these efforts are the beginning of the Network’s efforts to close the gap in healthcare outcomes along racial lines.