What is RSV (Respiratory Syncytial Virus)?
- Home
- |
- Health A to Z –...
- |
- Respiratory Syncytial Virus – RSV
Respiratory viruses are a part of life. They can be especially common in children under 5 and older adults with weakened immune systems. Most cases are mild, but for some, the symptoms could actually be respiratory syncytial virus (RSV).
RSV is a common respiratory virus. By the time children are 2 or 3 years old, most have been infected by RSV at least once, with few problems. For some, the virus can be life-threatening. An estimated 58,000-80,000 U.S. children younger than 5 years old are hospitalized with RSV, more than any other condition. Between 100 and 300 children die each year from RSV.
For U.S. adults ages 65 and older, an estimated 60,000-160,000 are hospitalized with RSV each year. Between 6,000 and 10,000 die due to RSV infection each year.
What causes RSV?
RSV is caused by the respiratory syncytial virus. Infection occurs through exposure to droplets of the virus or contact with an infected surface.
Is RSV contagious?
RSV is very contagious. It can be spread through droplets from an infected person’s cough or sneeze. The virus also lives on surfaces, so touching something like a doorknob and then touching your face can also spread the disease.
How long is RSV contagious?
Most people with RSV are contagious for 3 to 8 days. However, some infants and people with weakened immune systems can spread the virus for as long as 4 weeks.

RSV symptoms
Symptoms of RSV typically develop within 4 to 6 days of infection. The symptoms don’t appear all at once, but in stages. Parents and caregivers of children with asthma, premature infants, and elderly people need to be vigilant during RSV season. Learn to recognize the warning signs and seek medical treatment as soon as possible.
RSV symptoms include:
- Runny nose
- Decrease in appetite
- Coughing
- Sneezing
- Fever
- Wheezing
RSV in infants
Infants are the most seriously affected by RSV. In the youngest infants, symptoms may only be irritability, decreased activity, and breathing difficulties.
RSV starts as an upper respiratory infection, with familiar cold symptoms. What makes it so dangerous is its ability to quickly spread down from the nose and throat into the lower respiratory tract. From there it infects and causes inflammation in the tissues of the lungs (causing pneumonia) and the tiny bronchial air tubes (causing bronchiolitis).
Inflammation is the body’s natural process for fighting infection. But in tiny infant airways or those already inflamed by asthma, it can cause increased airway obstruction and difficulty breathing.
Another danger of RSV is that a serious RSV infection in young children increases the child’s risk of developing asthma in later years. Researchers do not know exactly why this happens. It may be a cause-and-effect reaction. The RSV infection may damage the lung, which leads to asthma. Or it may just be an association, where factors that put children at risk for asthma also put them at risk for a more serious RSV infection. RSV and other viruses have also been linked to an increased risk of sensitization to allergens and development of allergies.
How does a baby get RSV?
Babies can be exposed to RSV in a variety of settings, but daycare is a common source.
- Germs get into the child’s nose, mouth, or eyes either through the air or direct contact with germ-laden hands, toys or eating utensils.
- The germs settle in the upper respiratory tract: nose, eyes, sinuses, mouth, and upper throat.
- When the immune system is working efficiently, the sticky mucus that lines your nasal passages and sinuses traps the germs. The tiny hairs, called cilia, sweep germs out of the airways.
- If germs take hold and infection sets in, your immune system sends extra blood cells to the nasal passages, leaving them swollen, inflamed, and congested. At the same time, the nose produces extra mucus, which can overwhelm the cilia’s ability to clean things out – and leave you with a stuffed-up or runny nose.
- From the nose, germs can spread and cause infection in ears and sinuses. Or the germs move down into the large and small airways of the lungs and trigger asthma or lower respiratory tract infections.

When to take a baby with RSV to the hospital
While many cases of RSV can be treated at home, sometimes the illness is more severe requiring hospitalization. An estimated 58,000 children under the age of 5 are hospitalized every year with RSV.
Those most vulnerable include:
- Premature infants
- Very young infants, especially those 6 months and younger
- Children younger than 2 years old with chronic lung disease or congenital (present from birth) heart disease
- Children with weakened immune systems
- Children who have neuromuscular disorders, including those who have difficulty swallowing or clearing mucus secretions
Call 911 or take your child to the emergency room for any of these symptoms:
- Wheezing (noisy breathing when exhaling)
- Signs of trouble breathing nostrils widening with each breath; rapid breathing; skin above or below the ribs sucking in with each breath; skin, lips or nails turning blue
- A severe headache behind or around the eyes or the back of the neck; swelling or redness around the eyes
- Persistent vomiting or signs of dehydration: dry or sticky mouth; few or no tears; thirst; discolored or less urine than usual.

What is RSV Infographic Transcript
What is RSV?
RSV is a common respiratory virus. By the time children are 2 or 3 years old, most have been infected by RSV at least once, with few problems. However, for some, the virus can be life-threatening – and the infection sends more babies to the hospital than any other condition.
Who are high-risk people for RSV?
- For some, the virus can be life-threatening. High-risk groups include:
- Premature babies in first year of life
- Infants under 6 months
- Children with asthma
- Patients of any age with a weakened immune system or underlying lung or heart problems
Infants are most severely affected by RSV. Signs and symptoms of severe RSV infection in infants include:
- Short, shallow, and rapid breathing
- Struggling to breathe — chest muscles and skin pull inward with each breath
- Cough
- Poor feeding
- Unusual tiredness
- Irritability
- Fever – (temperature above 100 degrees Fahrenheit). Fever may not always be present
Adults/Older Children:
- Congested or runny nose
- Dry cough
- Low-grade fever
- Sore throat
- Sneezing
- Headache
RSV infection can spread to the lower respiratory tract, causing inflammation of the small airway passages entering the lungs. These signs include:
- Fever
- Severe cough
- Wheezing
- Rapid breathing or difficulty breathing
- Bluish color of the skin due to lack of oxygen (cyanosis)

RSV in toddlers
By the age of 2 most toddlers will have had RSV at least once. Yet, toddlers can become reinfected. For toddlers with chronic lung diseases, compromised immune systems, or neuromuscular disorders, it is important to remain vigilant.
Can adults get RSV?
RSV is also common among adults. Those at high risk for severe RSV include adults ages 65 and older, people with asthma or COPD, people with heart disease, cancer patients or people with an immunodeficiency or autoimmune disease. Also vulnerable to infection are people in close contact with large numbers of people, such as senior citizens living within group settings.
When is RSV season?
RSV season in the United States occurs during the fall, winter, and spring. In 2021, there was an unusual earlier RSV spike, beginning over the summer. This was due to the COVID-19 mitigation efforts in the 2020-2021 fall and winter.
How long does RSV last?
RSV symptoms typically last a few days to a few weeks. For many people, these symptoms may just appear like a common cold, but it can be more severe for some.
RSV testing
There are several tests available that can confirm a diagnosis of RSV. However, doctors often diagnose RSV based upon symptoms. But, if an infant, young child, or older adult has serious symptoms of an infection, a doctor may perform testing to confirm RSV.
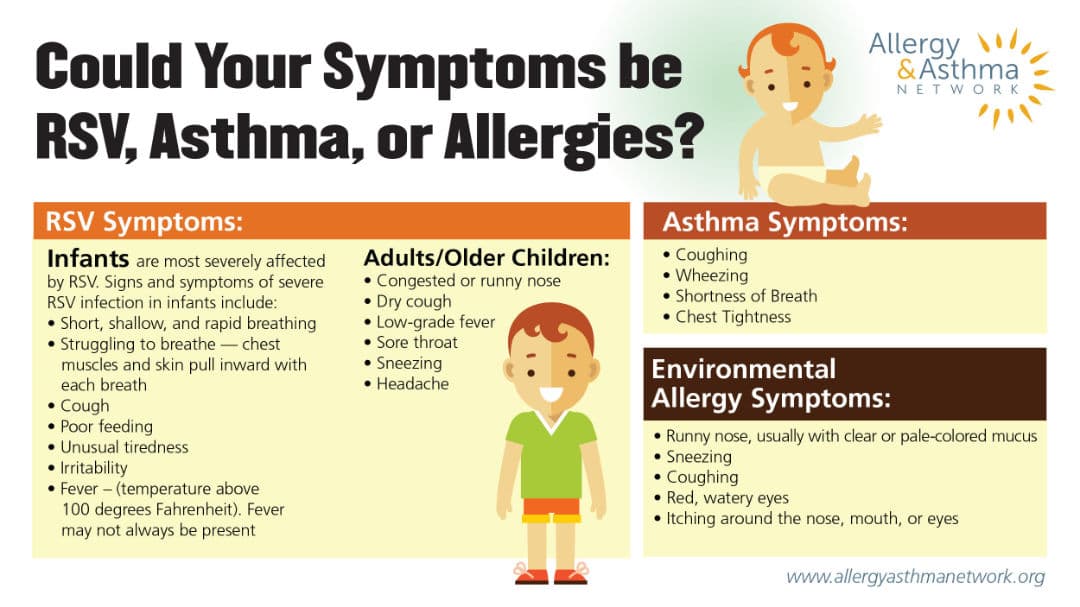
RSV, Asthma, or Allergies Infographic Transcript
Could Your Symptoms be RSV, Asthma, or Allergies?
RSV SYMPTOMS:
Infants are most severely affected by RSV. Signs and symptoms of severe RSV infection in infants include:
- Short, shallow, and rapid breathing
- Struggling to breathe — chest muscles and skin pull inward with each breath
- Cough
- Poor feeding
- Unusual tiredness
- Irritability
- Fever – (temperature above 100 degrees Fahrenheit). Fever may not always be present
Adults/Older Children:
- Congested or runny nose
- Dry cough
- Low-grade fever
- Sore throat
- Sneezing
- Headache
ASTHMA SYMPTOMS:
- Coughing
- Wheezing
- Shortness of Breath
- Chest Tightness
ENVIRONMENTAL ALLERGY SYMPTOMS:
- Runny nose, usually with clear or pale-colored mucus
- Sneezing
- Coughing
- Red, watery eyes
- Itching around the nose, mouth, or eyes

RSV vs cold
For many children and adults, RSV may appear just like a common cold. And, unless a person is specifically tested for RSV, they many never know they had it. But it isn’t “just a cold” and may be a more serious case of RSV.
Contact your child’s doctor if common cold symptoms are complicated by any of the following:
- The child is younger than three months
- The child has ever been diagnosed with asthma or reactive airways disease
- The child has a fever
- above 100.4° in babies under 3 months old
- above 101° in babies 3-6 months
- above 102° in babies older than 6 months
- Daytime cough or cold symptoms last for more than 10 days
- Cold symptoms come back a day or two after they seem to go away
- Tugs at an ear and develops an earache
- Wheezing with breathing
- Unusual irritability or less active
- Cough with colored sputum (yellow, green, grayish)
- Difficulty breathing or pauses in breathing (called apnea)
- Refuses to eat
- Shows signs of dehydration (no tears with crying, no wet diapers for 6 or more hours, or cool dry skin).
How does RSV spread?
RSV is a highly contagious virus. It is spread through inhaling droplets (such as from a cough or sneeze) from an infected person. It can also be spread through contact with infected surfaces.
RSV treatment
There is no medical cure for RSV. Physicians focus instead on treatments that reduce congestion and open the airways so the patient can breathe. Serious cases require hospital care, intravenous fluids, nebulizer medications and oxygen treatments.
Some patients get secondary pneumonia as a result; this needs to be treated aggressively with antibiotics. Some transplant patients with severe disease may benefit from adding an antiviral agent – but the primary treatment is supportive care.
RSV treatment babies
Treatment for RSV is largely supportive care to ease symptoms. It includes:
- managing fevers with over-the-counter fever reducers (check age ranges for dosage instructions);
- drinking plenty of fluids;
- suctioning mucus for young children who cannot blow their nose;
- taking a bath or sponge bath with lukewarm (not cold) water.
If symptoms cannot be managed at home, the baby needs to be hospitalized. Serious cases require hospital care, intravenous fluids, nebulizer medications and oxygen treatments.
Some high-risk babies may qualify to receive a preventive medicine called palivizumab, given by injection every month during RSV season. Palivizumab is not a vaccine.
How to treat RSV in toddlers
Treatment for RSV in toddlers is similar to babies. Make sure to keep the fever under control and provide plenty of fluids. If symptoms do not improve at home, seek medical care.
RSV prevention tips
RSV vaccines are expected to arrive in fall 2023. Two vaccines are available for adults ages 60 and older. An RSV monoclonal antibody, which acts similarly to a vaccine, is available for infants and young children. The vaccines are designed to prevent severe or life-threatening RSV symptoms. Vaccines for pregnant women and other age groups are coming soon.
Certain lifestyle changes can help protect you and your family from RSV. The virus can live on hard surfaces such as doorknobs and tabletops for days. It can spread quickly through human contact, often before the infected person shows any obvious signs of the disease.
To help prevent RSV:
- Wash hands frequently, especially before eating or before handling babies
- Wash and disinfect toys, tabletops, doorknobs, and other shared surfaces
- Avoid sharing cups, eating utensils or food
- Avoid people with obvious cold symptoms
- Avoid cigarette smoke, which can increase the risk of infection and severity of symptoms
- Don’t let others handle your baby without washing their hands

How to Wash Your Hands Infographic Transcript
How to Wash Your Hands
- Palm to Palm
- Back to Hands
- Between Fingers
- Back of Fingers
- Base of Thumbs
- Fingernails
- Wrists
Issues for Babies with RSV: Insurance
Most young children get respiratory syncytial virus, or RSV, before age 2. Parents of premature infants whose health insurance plans don’t cover preventive RSV treatment may suffer – and unnecessarily so. Video courtesy of National Coalition for Infant Health.
See Related Pages
- What is Chronic Rhinosinusitis with Nasal Polyps (CRSwNP)?
- Respiratory Syncytial Virus – RSV
- AERD: Aspirin Exacerbated Respiratory Disease
- Type II Inflammation Patient Navigator
- What is Chronic Urticaria?
- Allergic March
- Alpha-1 Antitrypsin Deficiency
- Bronchiectasis
- Celiac Disease
- COPD
- Coronavirus | COVID-19 Information
- Eosinophilic Esophagitis
- Food Intolerance vs. Food Allergy
- FPIES – Food Protein-Induced Enterocolitis Syndrome
- GERD – Gastroesophageal Reflux Disease
- Hereditary Angioedema
- Immunotherapy for Allergies
- Infections and Viruses
- Interstitial Lung Diseases
- Mast Cell Diseases
- Nasal Polyps
- Oral Allergy Syndrome (OAS)
- PANDAS – Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections
- Primary Immunodeficiency Diseases (PIDD)
- Psoriasis
- Pulmonary Hypertension
- Sinusitis
- Shared Decision Making
- Sleep Apnea
- VCD – Vocal Cord Dysfunction
Reviewed by:
Purvi Parikh, MD, FACAAI is an adult and pediatric allergist and immunologist at Allergy and Asthma Associates of Murray Hill in New York City. She is on faculty as Clinical Assistant Professor in both departments of Medicine and Pediatrics at New York University School of Medicine.
