COVID-19 Information Center
- Home
- |
- Health A to Z –...
- |
- Coronavirus | COVID-19 Information
We know COVID-19 is a serious concern for you if you have asthma, allergies or related diseases. Right now, experts are learning more about the coronavirus every week. We want to make sure you have the most current, accurate and trustworthy information to manage your health.
Check here weekly for updated information and news webinars, fact sheets, podcasts and infographics to help you.
Recent Covid-19 Updates
The COVID-19 pill is considered a major step forward in managing COVID-19. Two COVID-19 antiviral pills are currently available. Updated: January 5, 2024
What you need to know about COVID-19 risk, asthma and allergies if you host or visit relatives during the holidays.
How to Stay Safe on Halloween with Asthma and Allergies
Learn how you can minimize risk and maximize safety at Halloween when you have a child with a food allergy, asthma or latex allergy.
Why Getting the Flu Shot Is Critical for People with Asthma
If you have moderate to severe asthma, learn why getting your flu shot is especially important due to the ongoing COVID-19 pandemic.
Albuterol in Short Supply? Here’s What to Do
April 4, 2023 The ongoing shortage of liquid albuterol appears to be improving. Hospitals and...
Is It Fall Allergies or COVID-19? How to Tell the Difference
Learn how to tell the difference between fall allergy symptoms or COVID-19 symptoms.
COVID-19 Omicron Variants
Learn about COVID-19 Omicron variants of concern: symptoms, severity, prevention and treatment.
What It Means When COVID-19 Becomes Endemic
When the pandemic is officially over, what’s next? Medical experts say we will enter an endemic phase – similar to the flu. COVID-19 will still be present, but it will not disrupt everyday life.
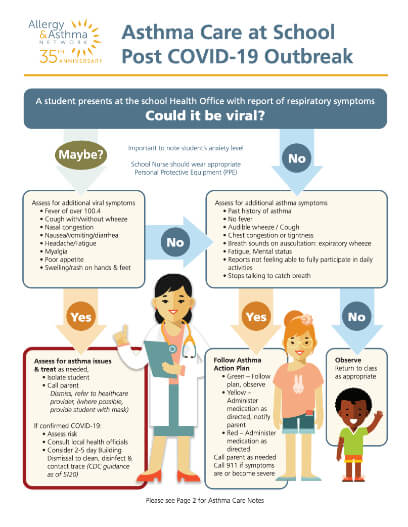
Asthma and COVID-19
Understanding the relevant content about COVID-19 and asthma that Allergy and Asthma Network has published over the course of the pandemic.
Vaccines and COVID-19: Science-based Thoughts on the Long-Haul (Recording)
This Webinar was recorded on Thursday, February 17, 2022. We review the latest vaccine information and look at the Long Haul effects of the COVID-19 virus.
Egg Allergy and Covid Vaccine
This “Ask the Allergist” video addresses both COVID-19 and flu...
COVID-19 and Immunity Issues: Current Treatment Options (Recording)
In this Free Webinar we look at COVID-19’s huge impact on people with secondary immune deficiencies and outline treatment issues.
COVID-19 Webinars ➛
Free & On-Demand
Frequently Asked COVID-19 Questions
Are people with asthma at greater risk for catching COVID-19?
People with asthma are not believed to be at higher risk of getting infected with COVID-19 — but if you do get infected you may be at higher risk of getting very sick.
COVID-19 can:
- affect your respiratory tract (nose, throat, lungs)
- cause an asthma attack
- possibly lead to pneumonia and acute respiratory disease.
Are people with asthma at high risk of severe illness if they get COVID-19?
CDC says adults of any age with moderate to severe asthma may be at increased risk for severe illness from COVID-19.
However, many studies examining the relationship between asthma and COVID-19 have found no increased risk of severe illness or complications, according to the American Academy of Allergy, Asthma & Immunology (AAAAI).
A few studies have revealed nonallergic asthma may be linked to more severe illness from COVID-19, AAAAI says. These studies are not conclusive, however, as it’s not clear if the patients had COPD, a known risk for severe cases of COVID-19.
What’s the takeaway for people with asthma? Keep your asthma under the best possible control at all times, take your daily controller medications as prescribed and follow your Asthma Action Plan. That way your lungs will be healthy and well prepared to fend off any virus or infection.
How do I find out when I can get a COVID-19 vaccine?
Vaccines are now widely available in all U.S. states. They are available for all adults and children ages 12-18. Here is how find a vaccination site near you:
- Visit Vaccine.gov to find a location near you.
- Check your local pharmacy’s website to see if vaccination appointments are available.
- Call your state or county health department to find vaccination sites in your area.
Widespread vaccination is a critical tool in stopping the pandemic.
What are recommendations for people with asthma?
More than 24 million people in the United States have asthma and 10 people die from asthma in the United States daily. It is important to practice COVID-19 prevention strategies if you have asthma due to the increased risk of severe complications.
If you have asthma, be sure to continue to follow your Asthma Action Plan or treatment plan.
Additional things you can do:
- Get the COVID-19 vaccine to protect yourself and others. Visit Vaccine.gov to find a location near you.
- Know how to use your inhaler correctly.
- Avoid your asthma triggers.
- Clean and disinfect frequently touched surfaces like tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets and sinks daily to protect yourself against COVID-19.
- Avoid disinfectants and scented hand sanitizers that may cause an asthma attack.
- Take your asthma medication exactly as prescribed.
- Talk to your healthcare provider, insurer and/or pharmacist about creating an emergency supply of prescription medications such as asthma inhalers. There is no need to hoard medications.
- Make sure that you have 30 days of nonprescription medications and supplies on hand in case you need to stay home for a long time.
Who is at the greatest risk for severe COVID-19 complications?
Some people are at higher risk of getting very sick from COVID-19. These groups include:
- Older adults, with risk increasing by age.
- People who live in a nursing home or long-term care facility.
- Pregnant women.
- People of any age with certain underlying medical conditions are at increased risk for severe illness from COVID-19:
- Chronic kidney disease
- COPD
- Weakened immune system from solid organ transplant
- Obesity (body mass index of 30 or higher)
- Heart conditions including coronary artery disease or cardiomyopathies
- Sickle cell disease
- Type 2 diabetes
People with the following conditions might be at increased risk for severe illness from COVID-19:
- Asthma (moderate to severe)
- Pulmonary fibrosis (damaged or scarred lung tissue)
- Weakened immune system from immune deficiencies, HIV, use of corticosteroids or other immune weakening medications and blood or bone marrow transplant
- Smoking
- Cystic fibrosis
- Hypertension or high blood pressure
- Cerebrovascular disease (affects blood vessels and blood supply to brain)
- Neurologic conditions such as dementia
- Liver disease
- Thalassemia (a type of blood disorder)
- Type 1 diabetes
Research is ongoing involving whether asthma is a risk factor for more severe complications from COVID-19. While CDC says it MAY be a risk for more severe COVID-19, other studies suggest it is NOT a risk factor.
Several studies indicate people who have nonallergic asthma – symptoms caused by something other than allergies, such as exercise, air pollution, weather conditions or stress – may be at increased risk for severe COVID-19 compared to those with allergic asthma.
Should I wear a face mask?
CDC face mask guidelines are based on levels of COVID-19 in each community. The levels are determined by the total number of people with COVID-19 admitted to the hospital; hospital beds in use; and the total number of new COVID-19 cases in the area.
CDC lists three levels to determine whether face masks are appropriate in a community. This applies to adults and children ages 2 and older. It also applies regardless of vaccination status.
HIGH –You should wear a mask indoors in public places (including K-12 schools and other community settings). This may be especially important for people who are immunocompromised or at high risk for severe illness. People who are immunocompromised or at high risk for severe illness may include people with moderate to severe asthma, COPD or other chronic lung diseases.
MEDIUM – You can choose to wear a face mask based on your personal preference or personal risk assessment. However, if you are immunocompromised or at high risk for severe illness, talk with your doctor about whether to wear a mask indoors. If you live with someone at high risk for severe illness, consider wearing a mask when indoors with that person.
LOW – You can choose to wear a face mask based on your personal preference or personal risk assessment.
Check your community’s level and locate areas of the country with high levels on CDC’s website.
There is no evidence that wearing a face mask can worsen your asthma, according to the American College of Allergy, Asthma & Immunology. However, some people with moderate to severe asthma may feel it is more difficult to breathe while wearing a face mask. If you don’t feel you can wear a mask due to your asthma, it may be best for you to stay home or avoid public places as much as possible. Ask family and friends to run errands for you. If you must go out, avoid large crowds and practice social distancing. Being in public without a face mask may increase your chances of getting COVID-19 or passing it on to others.
How is COVID-19 transmitted?
COVID-19 can be spread from person to person. Similar to other colds and viruses, it spreads primarily by close contact with someone who is infected. Research reveals that COVID-19 can be spread by people who are not showing symptoms.
Transmission can happen when respiratory droplets produced when an infected person coughs, sneezes or talks and the virus is released into the air. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. Droplets generally don’t travel more than a few feet before they fall to the ground, but there are cases – especially indoors and in places with poor ventilation – where they may travel further or linger in the air.
CDC defines “close contact” as spending a total of 15 minutes or more within 6 feet of someone who is infectious with COVID-19. The 15 minutes does not have to consecutive; it can occur in a series of brief encounters. It’s believed people need to be exposed to a certain level of the virus in order to get infected; the more exposure, the higher the level of the virus and the more likely people are to get COVID-19.
The risk of COVID-19 transmission indoors is highly variable – it can depend on the size of the respiratory droplets and the airflow in the room. The risk of transmission outdoors is safer than indoors, but there are cases of transmission in crowded outdoor locations.
The U.S. Centers for Disease Control and Prevention (CDC) recommends social distancing, in which we stay at least 6 feet apart from other people, and that we wear face masks when around other people.
COVID-19 can also be spread by touching a contaminated surface or object. (A cell phone or computer keyboard and mouse, for example, are items that can be contaminated with COVID-19.) The virus can be transmitted if you then touch your mouth, eyes or nose.
Is COVID-19 airborne?
COVID-19 most commonly spreads through close contact with an infected person, however according to CDC there is evidence that in certain conditions, it may spread via respiratory droplets to people further than 6 feet away from the person who is infected. The virus may also linger in the air after the infected person has left, potentially infecting those still in the space.
This is called airborne transmission. CDC updated its COVID-19 guidance on Oct. 5 to reflect this assessment.
Transmissions that infect people who are further than 6 feet away have occurred in indoor spaces that have poor ventilation. It could be the infected person was speaking loudly, singing or breathing heavy after exercise.
To avoid exposure and minimize the risk of airborne transmission when indoors, CDC recommends staying at least 6 feet away from others whenever possible, avoid crowded indoor spaces and to cover your mouth and nose with a face mask when around others.
Why is there so much concern about COVID-19?
Cases of COVID-19 and instances of community spread are reported in all states. Community spread means some people have been infected and it is not known how or where they became exposed to the virus. People in places where there is ongoing community spread of COVID-19 are at higher risk of exposure, with the risk level dependent on your location, according to CDC.
This is a health situation that continues to evolve. CDC also notes the following:
- Healthcare workers caring for patients with COVID-19 are at elevated risk of exposure.
- Close contacts of persons with COVID-19 also are at elevated risk of exposure.
- Travelers returning from affected international locations where community spread is occurring also are at elevated risk of exposure, with increase in risk dependent on location.
In addition, certain people are at higher risk for severe illness and death from COVID-19, according to CDC:
- People 65 years and older
- People who live in a nursing home or long-term care facility
- People of all ages with serious underlying medical conditions
What are the symptoms of COVID-19?
Symptoms vary in severity. Many cases are mild, but some are severe and life-threatening – usually in people who have some type of compromised immunity.
Primary symptoms:
- Fever
- Cough
- Shortness of breath or difficulty breathing
- Chills (sometimes with shaking)
- Sore throat
- Fatigue
- Congestion or runny nose
- Muscle or body aches
- Headache
- Nausea or vomiting
- Diarrhea
- A loss of taste or smell
Some people diagnosed with COVID-19 experience small, itchy blisters or hives with flat and raised lesions. Others report purple skin marks, rashes or lesions on their toes (and sometimes fingers). Labeled “COVID toes,” sometimes they appear before COVID-19 symptoms begin; sometimes they appear with no other symptoms. Doctors believe they are related to the virus attacking blood vessels. Skin symptoms and COVID toes tend to go away within 10-14 days.
What do I do if I’m feeling sick with COVID-19?
If you suspect you may have COVID-19, please stay home and minimize contact with other people. You should call your doctor and discuss your symptoms and potential exposure. Your doctor will decide whether you need to be tested. You may also ask to be tested for COVID-19 by contacting a local health department.
Most people who are mildly ill may need to just self-isolate at home until the virus runs its course.
Other important measures if you are sick:
- Wear a facemask when around other people if instructed to do so by your doctor.
- Separate yourself as much as possible from other people in your home
- Cover your cough and sneezes, or cough into your elbow
- Wash your hands often
- Don’t share objects
When should I seek immediate medical attention?
If you have any of these emergency warning signs for COVID-19, get medical attention immediately:
- Trouble breathing
- Persistent pain or pressure in the chest
- Feeling confused or not able to arouse
- Bluish lips or face
- Inability to wake or stay awake
Call 911 if you have a medical emergency. Notify the operator that you have, or think you might have, COVID-19. If possible, put on a cloth face covering before medical help arrives.
COVID-19 is a specific coronavirus that emerged in late 2019. It can cause severe symptoms in some people. The COVID-19 virus has spread globally and is now a pandemic.
What COVID-19 prevention strategies are recommended by CDC?
CDC continues to recommend avoiding large events and gatherings in order to reduce risk of getting or spreading the COVID-19 virus.
Preventive measures are the same as what’s recommended to avoid the flu or the common cold:
- Get the COVID-19 vaccine to protect yourself and others. Visit Vaccine.gov to find a location near you.
- Wash your hands often with soap and water, especially after going to the bathroom, before eating and after blowing your nose, coughing or sneezing.
- Put distance between yourself and other people (at least 6 feet) if COVID-19 is spreading in your community. This is especially important for people who are at higher risk of getting very sick.
- Use an alcohol-based hand sanitizer with at least 60 percent alcohol if soap and water are not immediately available.
- Avoid touching your mouth, eyes or nose.
- Avoid sharing anything – including cups, water bottles and eating utensils.
- Disinfect all frequently touched surfaces.
- Avoid close contact with people who are sick.
How long does it take for symptoms to appear once infected with COVID-19?
Why is COVID-19 considered a pandemic?
COVID-19 has spread worldwide and the World Health Organization (WHO) has declared it a pandemic. Pandemics occur when a new virus emerges to infect people and spread because there is little to no pre-existing immunity to it.
How do I manage stress due to COVID-19?
As more cases of COVID-19 are discovered and our communities take action to combat the spread of disease, it is natural for some people to feel concerned or stressed. Strong emotions can trigger an asthma attack. Take steps to help yourself cope with stress and anxiety.
Here’s advice on managing your mental health, stress and anxiety during the COVID-19 pandemic.
What do I do if I am unable to obtain an albuterol inhaler?
In March 2020, certain areas of the United States experienced a shortage of albuterol quick-relief inhalers. This occurred due to supply chain issues and increased use of albuterol inhalers in hospitals to treat COVID-19 patients. Manufacturers have since resupplied pharmacies and, as of October 2020, the shortage has largely been resolved.
If you are unable to fill your asthma inhaler prescription for any reason, there are options available. These include:
- Contact your allergist or primary care doctor – other inhaler options are available.
- Visit GoodRx.com to search for other pharmacies in your area that may be able to fill your prescription.
- If you can’t afford your asthma medication, refer to this list of patient assistance programs and discount cards to help with the cost.
- Follow your Asthma Action Plan and avoid your asthma triggers to prevent flare-ups that require quick-relief medication.
- Remember to not overuse your albuterol inhaler. One canister should last for months. If you’re using your albuterol inhaler more than twice a week to relieve symptoms, that’s a sign your asthma may not be well controlled, and you should schedule an appointment to see an allergist.
Is there a COVID-19 treatment available?
Promising treatments are available for people who get sick with COVID-19.
One is monoclonal antibody infusion therapy. Monoclonal antibodies are given intravenously as infusion therapy before patients need hospitalization. This therapy uses COVID-19 antibodies to help a person’s body fight off the infection. Research suggests the antibodies lower the amount of virus — the “viral load” — in a person’s body. This can help prevent hospitalization and death.
FDA has granted emergency use authorization to sotrovimab, a monoclonal antibody treatment that prevents the COVID-19 virus from entering the body’s cells. Sotrovimab is proving effective against some COVID-19 variants.
Treatments are also available for people hospitalized with COVID-19. In October 2020, the U.S. Food and Drug Administration (FDA) approved remdesivir for use in hospitalized adults and children 12 years of age or older who weigh at least 88 pounds. Remdesivir, a broad spectrum anti-viral medication, is only administered in a hospital setting or a healthcare facility able to provide acute patient care.
In 2021, two COVID-19 pills received emergency use authorization from FDA. One is molnupiravir (brand name Lagevrio™). The other is Paxlovid™, a combination of nirmatrelvir and the HIV drug ritonavir. Research shows both medications are effective in preventing hospitalizations and death from COVID-19 infection.
Another COVID-19 treatment is dexamethasone, a type of corticosteroid. It’s used in hospitalized patients who are using ventilators to support breathing or require supplemental oxyten. It is recommended by the National Institutes of Health’s COVID-19 Treatment Guidelines Panel.
What is the impact of COVID-19 on people of color?
Racial inequities are central to the national conversation about COVID-19. CDC data reveals the rate of Black Americans, Native Americans and Hispanic/Latino communities who are hospitalized or die from COVID-19 is significantly higher than other races.
Inequalities in healthcare that existed before the pandemic have worsened during the COVID-19 pandemic. Communities with majority Black and Hispanic populations face limited access to medical care and treatment. There are often fewer COVID-19 testing sites in these communities as well. Some live in substandard or overcrowded housing and are employed in front-line occupations, putting them at higher risk of COVID-19 exposure.
The presence of underlying conditions, including asthma, obesity, heart disease and diabetes, may worsen COVID-19 symptoms.
Allergy & Asthma Network is working with partners to provide community-based health screenings and education so we can better address health disparities impacting underserved communities. The Not One More Life Trusted Messengers program offers free COVID-19, asthma and COPD online health screenings and telehealth support.
Learn more about racial inequities in healthcare here and uncover the path to achieving health equity.
What are COVID Long Haulers?
Some people continue to experience COVID-19 symptoms after the infection has passed and testing is negative. Sometimes these long-haul symptoms last for months. They often affect daily lives and the ability to work.
The National Institutes of Health reports between 10-30% of people infected with COVID-19 experience long-term symptoms.
Long-haul symptoms may include:
- Coughing
- Fatigue
- Body aches and joint pain
- Shortness of breath
- Loss of taste or smell
- Sleep problems
- Nausea
- Inability to concentrate
- Confusion
- Memory problems
- Some long-term issues become serious. Long haulers are reporting kidney problems, onset of diabetes, lung damage including scarring, and clotting issues that can lead to a heart attack or stroke.
Long-haul symptoms can occur in people who developed severe COVID-19 illness or had no symptoms at all. Learn more in our COVID-19 Long Haul post.
Free COVID-19, Asthma, COPD screenings and digital health support —>
Covid-19 Infographics


Remember the 3 W’s: Wash Your Hands, Watch Your Distance, Wear a Mask
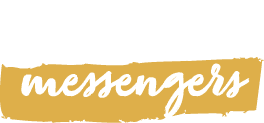
School

Business

Spanish


Tools to Regulate Mind, Body and Emotions during COVID-19

Videos Related to COVID-19
Allergy & Asthma Network’s COVID-19 Conference Series
Black People Like Me Virtual Conference Series
Black People Like Me is a series of six online events. It is a a conversation with the Black community to better understand and address the impact of asthma and COVID-19 on the Black community.
Unidos Hablemos de… Asthma & COVID-19 Conference
‘Unidos Hablemos de…’ was a series of six monthly virtual events held from October 2021 to March 2022. We connected with people from the Hispanic and Latino community to address asthma and COVID-19.
Unidos Hablemos de… Conferencia sobre el asma y el COVID-19
“Unidos hablemos de…” fue una serie de seis eventos virtuales mensuales que se llevaron a cabo entre octubre de 2021 y marzo de 2022. Estos eventos se presentaron en español e inglés.















