Asthma and COVID-19
Published: November 3, 2025 Revised: November 5th, 2025

COVID-19 is caused by the SARS-CoV-2 virus. It is a respiratory illness that emerge in late 2019 and quickly spread across the world. The virus primarily affects the lungs and airways. It causes symptoms that range from mild cold-like congestion to severe pneumonia and breathing difficulties.
How does COVID-19 impact people with asthma, a chronic lung disease?
Studies show that most people with well-controlled asthma are not at higher risk of getting COVID-19 or developing severe illness. However, people with moderate to severe asthma may be at higher risk of getting very sick from COVID-19. The key factor appears to be the level of asthma control. Keeping symptoms stable plays an important role in reducing risk from respiratory infections.
The best way to prevent severe COVID-19 outcomes? Get the COVID-19 vaccine.
Here is what you need to know about COVID-19 and asthma:
What are COVID-19 symptoms?
COVID-19 symptoms can vary in severity. Many cases are mild. Some are severe and life-threatening. People with a respiratory disease or compromised immunity are often most impacted.
Primary symptoms include:
- Fever
- Chills (sometimes with shaking)
- Shortness of breath or difficulty breathing
- A dry cough
- Nasal congestion or runny nose
- Sore throat
- Fatigue
- Muscle or body aches
- Headache
- Nausea, vomiting or diarrhea
- New loss of taste or smell (in some people)
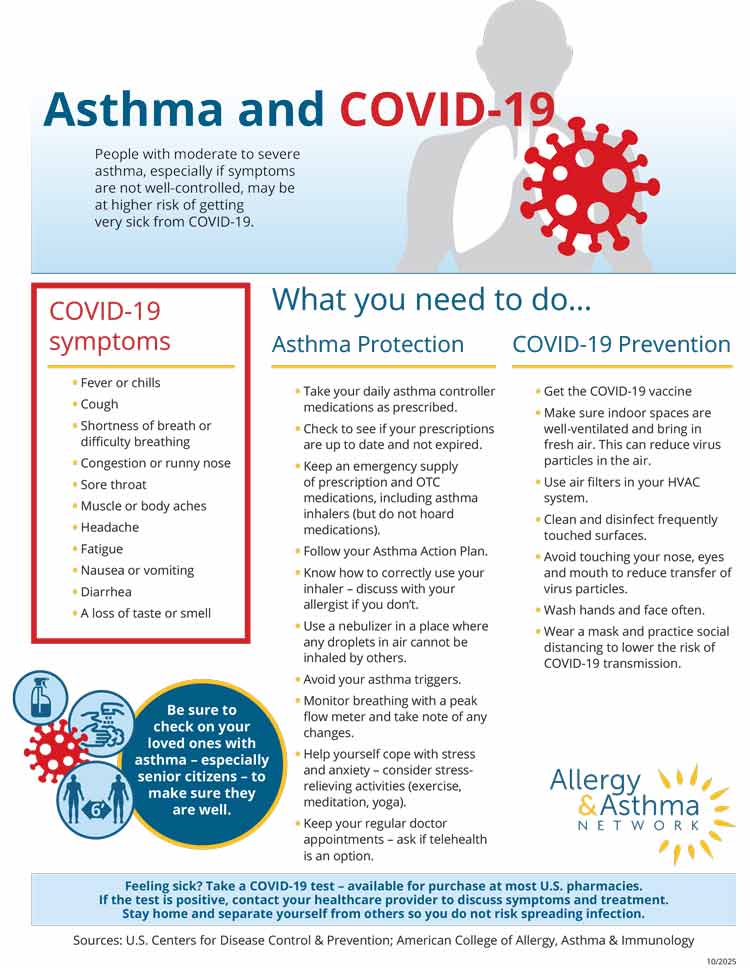
Download this infographic as a PDF
COVID-19 vs. asthma: how to tell the difference
In the age of COVID-19, if you develop a cough or shortness of breath it is often cause for alarm. You may wonder: “Do I have COVID-19 or is it my asthma acting up?”
Symptoms of COVID-19 and asthma do overlap somewhat. It’s important to take a look at the similarities and differences.
| COVID-19 | ASTHMA |
|---|---|
| Fever of over 100.4 | No fever |
| Dry cough, with or without wheeze | Cough and wheeze |
| Shortness of breath | Shortness of breath |
| Nasal congestion or runny nose | Chest tightness |
| Nausea/vomiting/diarrhea | Congestion |
| Headache | You have to stop talking to catch your breath |
| Fatigue | Fatigue |
| Muscle or body aches | Not able to perform daily activities |
| Not able to perform daily activities | |
| Loss of taste or smell in some people |
A COVID-19 respiratory infection may worsen asthma symptoms.
Are people with asthma at greater risk for getting COVID-19?
Asthma patients are not at higher risk of getting infected with COVID-19. But if they do get infected, they may be at higher risk of getting severe disease.
COVID-19 can:
- affect your respiratory tract (nose, throat, lungs);
- cause asthma exacerbations;
- possibly lead to bronchitis or pneumonia.
There is no evidence that common asthma medications – inhaled or oral corticosteroids, montelukast and biologics – increase your risk of getting COVID-19.
Are people with asthma at high risk of severe illness if they get COVID-19?
People with moderate to severe asthma, especially if the asthma is not well-controlled, may be at higher risk for severe illness from COVID-19, according to CDC. (This also includes people with chronic obstructive pulmonary disease, or COPD.)
The asthma data supporting this is not conclusive, however. There is no published study to confirm CDC’s assessment. A 2022 analysis of multiple COVID-19 findings suggest asthma doesn’t seem to make COVID-19 more severe or deadly.
Some studies suggest nonallergic asthma may be among risk factors for severe illness from COVID-19. These studies are also not conclusive. It’s not clear if the study participants also had COPD, a known risk for severe cases of COVID-19.
What’s the takeaway for asthma patients? Keep your asthma under the best possible control at all times. Take your daily controller medications as prescribed. Minimize any risk factor that can worsen asthma. Follow your Asthma Action Plan. That way your lungs will be healthy and well prepared to fend off any virus or infection.
What are recommendations for people with asthma to prevent COVID-19?
More than 28 million people in the United States have asthma. About 10 people die from the disease each day. It is important to practice COVID-19 prevention strategies if you have asthma. This is due to the potential for increased risk of severe illness.
What are COVID-19 prevention tips?
- Get the COVID-19 vaccine. Under 2025 guidance issued by CDC, all people 6 months of age and older, including adults 65 and older, are eligible to get the COVID-19 vaccine after consulting with a physician, nurse or pharmacist. The consultation should involve clinical shared decision-making that addresses the benefits and risks or COVID-19 vaccination. According to a CDC advisory panel that reviews vaccines, the risk-benefit of COVID-19 vaccination is most favorable for people who have at least one high-risk health condition (such as asthma). This would put them at increased risk for severe COVID-19. The risk-benefit is lowest for people not at increased risk.
- Wash your hands and face regularly. Avoid touching your nose, eyes and mouth.
- Disinfect frequently touched surfaces like tables, doorknobs, light switches, countertops, handles, desks, phones, keyboards, toilets, faucets and sinks daily.
- Make sure indoor spaces such as your home are well-ventilated and get fresh air. Open windows or doors, use fans, and use air filters in your HVAC system.
- If you have COVID-19, or you’re concerned about getting COVID-19, you may choose to wear a face mask and/or practice social distancing to lower the risk of transmission.
What are asthma management tips to help protect against COVID-19?
- Take your daily asthma controller medication as prescribed, even if you have well controlled asthma
- Use your quick-relief inhaler at the first sign of asthma symptoms.
- Keep your regular doctor appointments. Ask if telehealth is an option.
- Check to see if your prescriptions are up to date and not expired.
- Identify and avoid your asthma triggers.
- Get the flu vaccine before or during flu season.
- Minimize stress.
- Know how to correctly use your inhaler. Discuss this with your doctor if you don’t.
- Use a nebulizer in a place where any respiratory droplets in the air cannot be inhaled by others.
- Monitor breathing with a peak flow meter and take note of any changes.
Should I wear a face mask if I have asthma?
If you have asthma and getting a respiratory virus is a trigger for symptoms, you may want to consider wearing a face mask in public or group settings. Face masks can help lower your risk of getting COVID-19. They can protect you from breathing in respiratory particles infected with COVID-19. Masks also reduce the spread of the virus if you have COVID-19.
What face mask should you wear? Wear a face mask that is most comfortable for you. You may have to wear a face mask for long periods of time. So comfort is important.
The face mask should also be effective. Here’s what you need to know about the types of face masks available to the public:
- N95 and KN95 respirators – designed to protect against respiratory droplets in the air. They have 95% effectiveness. They also have exhalation valves that let air escape when you breathe out. This makes it easier to breathe.
- Barrier face covering – provides protection against respiratory droplets. They are less effective than N96 and KN95 respirators. They filter the air you breathe out, so you can wear them to protect others around you if you have COVID-19.
- Disposable face masks – may help block respiratory droplets in the air. It is unknown how effective these one-time-use masks are in terms of preventing infection. They are best used to protect others around you if you have COVID-19.
- Cloth face masks – may block respiratory droplets in the air. It is unknown how effective these one-time-use masks are in terms of preventing infection.
There is no evidence that wearing a face mask can worsen your asthma, according to the American College of Allergy, Asthma & Immunology (ACAAI).
What should you do if you think you have COVID-19?
First, take a COVID-19 test to confirm if you have it. At-home tests are available for purchase at most pharmacies and supermarkets. They can cost $10 to $20. You can also ask for a test at your doctor’s office. (Note: the federal government program that sends free at-home COVID-19 tests by mail has ended.)
If you have COVID-19:
- Call your doctor for guidance, especially if you are at high risk for severe symptoms.
- Consider a telehealth visit to talk with your doctor without leaving your home.
- Isolate yourself from others when possible.
- Wear a face mask to protect others around you.
- Clean commonly touched surfaces to prevent the spread of germs.
- If you are having trouble breathing, call 911. Be sure to tell them you have COVID-19.
If you are having asthma issues unrelated to COVID-19:
- Follow your Asthma Action Plan.
- Use your quick-relief inhaler and controller medications as prescribed.
- Call 911 if your symptoms become severe
Is it safe to use your asthma inhaler if you have COVID-19?
Yes, you can and should use your quick-relief and controller medications if you have COVID-19. Studies have shown these medications to be safe.nd controller medications. Studies have shown these medications to be safe.
How is COVID-19 treated?
Most people who are ill with COVID-19 will need to stay at home and get plenty of rest until the virus runs its course.
If you are at high risk of getting severe COVID-19 illness due to your asthma, contact your doctor or pharmacists about treatment options. Antiviral pills are available to treat COVID-19. They should be prescribed and started within 5–7 days after symptoms appear.
What is the COVID-19 antiviral pill?
Three antiviral medications are available to treat COVID-19 and prevent severe symptoms. Two are pills:
- Paxlovid® (nirmatrelvir and ritonavir) is fully approved by the U.S. Food and Drug Administration (FDA) for adults 18 years of age and older at risk for severe COVID-19 illness. This includes people with asthma. Paxlovid is also approved under an Emergency Use Authorization (EUA) for children ages 12-18 at risk for severe illness.
- Lagevrio® (molnupiravir) is approved under an EUA for adults 18 years of age and older at high risk for severe COVID-19 illness. It is not recommended for use by pregnant women.
The third is delivered by IV injection:
- Veklury® (remdesivir) is FDA-approved but can only be administered in a medical facility such as a hospital. It is for adults and children 12 years of age and older who weigh at least 88 pounds.
The antiviral pills are designed to prevent onset of severe COVID-19 symptoms and help reduce the risk of hospitalization and death.
Both Paxlovid and Lagevrio should be taken within five days of experiencing COVID-19 symptoms. The therapy can be taken at home, making this antiviral treatment ideal for many patients. The pills work by limiting the ability of the virus to replicate.
People with asthma should talk with their doctor about using their asthma medications while taking Paxlovid. Long-acting beta-agonists (LABA) taken with Paxlovid may cause heart risks. Salmeterol, in particular, may need to be withheld during Paxlovid treatment. Certain inhaled corticosteroids taken with Paxlovid may put patients at increased risk for Cushing’s syndrome and adrenal suppression.
In most cases, the benefits of a short course of Paxlovid to treat COVID-19 will outweigh the potential risks. It may be more dangerous to stop taking asthma medication even for a short period of time. That’s why it’s important to talk with your doctor about the risks and any possible alternative medications.
Should people with asthma get the COVID-19 vaccine?
Yes, says board-certified allergist and immunologist Purvi Parikh, MD, national spokesperson for Allergy & Asthma Network. The COVID-19 vaccine allows your body to develop a level of immunity to the virus.
All people 6 months of age and older are eligible to get the COVID-19 vaccine after consulting with a physician, nurse or pharmacist. The consultation should involve clinical shared decision-making. The discussion should address the benefits and risks of COVID-19 vaccination.on.
According to a CDC advisory panel that reviews vaccines, the risk-benefit of COVID-19 vaccination is most favorable for people who have at least one high-risk health condition. This would put them at increased risk for severe COVID-19. The risk-benefit is lowest for people not at increased risk.
The list of health conditions that put people at elevated risk for severe COVID-19 illness (this is not a complete list and it may change):
- Moderate to severe asthma
- COPD
- Bronchiectasis
- Pulmonary hypertension
- Scarred lung tissue
- Cancer
- Diabetes (Type 1 or Type 2)
- Heart disease
- Being overweight or obese
- Mental health conditions including depression
- Physical inactivity
Some U.S. states are issuing vaccine guidance separate from the federal government. Patients and healthcare providers should check with their state public health agency.
COVID-19 can be a very serious, life-threatening illness. The vaccines have been shown to be highly effective in preventing severe outcomes. They allow your body to develop immunity to the virus without getting sick. If someone who is vaccinated does get diagnosed with COVID-19, they are less likely to experience severe illness. Getting vaccinated protects people around you as well.
“I encourage everyone who is offered or has access to the vaccine to get it as soon as possible,” Dr. Parikh says.
How effective are COVID-19 vaccines?
Clinical trials show that people who have received COVID-19 vaccines are at lower risk of getting COVID-19 than people who are not fully vaccinated. They are also at lower risk of severe illness, hospitalization and death from COVID-19. They are also less likely to develop long COVID.
Getting sick with COVID-19 does provide a level of immunity, but how long varies from person to person. And the illness brings risk of severe symptoms or death. Thus, developing immunity through vaccination is the safest choice.
Remember, no vaccine is 100% effective. Viruses – especially COVID-19 – can mutate quickly. Different versions of a virus can emerge. You may still get sick from a circulating virus even if you get vaccinated. If you do get sick, the vaccines can help prevent severe symptoms, hospitalization and death.
What COVID-19 vaccines are available to people with asthma?
Three COVID-19 vaccines are available in the United States: the Pfizer, Moderna and Novavax vaccines. The Johnson & Johnson vaccine is not currently available in the United States.
Before CDC updated its guidance to include everyone 6 months of age and older (subject to shared decision-making), the U.S. Food and Drug Administration (FDA) approved COVID-19 vaccines for people at higher risk of severe illness. This includes people with asthma and other long-term health conditions. (While FDA approves vaccines for use, CDC gives guidance on who should get the vaccine and how it should be used.)
Here are the approved age ranges for each of the available vaccines:
- Pfizer is available for adults and children ages 5 years and older. It is no longer available for children under 5 years of age. FDA removed the vaccine’s emergency use authorization (EUA) for that age group.
- Moderna is available for adults and children ages 6 months and older.
- Novavax is available for adults and children ages 12 years and older.
No prescription is required to obtain a COVID-19 vaccine.
Pfizer and Moderna vaccines are Messenger RNA (mRNA) vaccines. Novavax is a protein vaccine.
- Messenger RNA (mRNA) vaccines. The mRNA vaccines do not contain the live virus. It contains a synthetic material that mimics the virus. This sends your body a message to produce antibodies and cells that build up an immune system defense. It can protect people from getting infected or severely sick when exposed to the real virus.
- Protein vaccines. Protein technology has been used for decades in vaccines, including those for hepatitis B and HPV. Novavax is a protein subunit nanoparticle vaccine. It is recombinant, meaning it’s made up of two different sources. Novavax introduces the harmless parts of the virus’s spike protein into the body. This leads to an immune response and builds up antibodies against the COVID-19 virus. It can protect people from getting infected or severely sick.
COVID-19 vaccines are available at doctor’s office and most pharmacies.
What are the side effects of the COVID-19 vaccines?
The COVID-19 vaccine may cause:
- Pain and/or swelling at the injection site.
- Fever
- Chills
- Fatigue
- Headache
- Nausea
- Muscle aches
- Joint pain
These symptoms are normal as the body works to build immunity to the virus.
Rare cases of myocarditis, pericarditis and severe allergic reactions have been reported post-vaccine. Myocarditis is inflammation of the heart muscles and the side effect appears to be more common in young males. Pericarditis is inflammation of the lining around the heart.
People who have had a severe allergic reaction to any of the COVID-19 vaccine ingredients should talk with their doctor before getting the vaccine. (Severe allergic reactions to vaccines are very rare.) The ingredients for each of the COVID-19 vaccines are on the FDA website. You and your doctor can decide together on whether it’s safe for you to get the vaccine. If you do not get the vaccine, talk to your doctor about alternative options for COVID-19 protection.
How can COVID-19 vaccine side effects be managed?
Not everyone will develop side effects from the COVID-19 vaccine. If you do have side effects, there are things you can do to minimize the symptoms:
- Use a cool, wet and clean towel over the injection site
- Move the affected arm
- For fever – drink lots of fluids and wear light clothing
Should people with asthma on inhaled or oral corticosteroids get the COVID-19 vaccine?
Yes, it is considered safe for people with asthma who take inhaled or oral corticosteroids to get the COVID-19 vaccine.
Inhaled corticosteroids (ICS) typically come in low or moderate doses. These medications should not weaken the immune system or reduce the effectiveness of the COVID-19 vaccine. It’s safe to get the vaccine while on ICS.
Oral corticosteroids (OCS) are a much higher dose but are still considered safe. However, some studies suggest that taking high-dose corticosteroids could weaken the immune system and might not provide strong or long-lasting protection. Your doctor may schedule your COVID-19 vaccine when you stop taking corticosteroids or your dose is at its lowest.
If you have any concerns about your asthma medications and the COVID-19 vaccine, speak with your doctor.
Should people with asthma on biologics get the COVID-19 vaccine?
Yes, it is safe for people who take biologic injections for asthma to get the COVID-19 vaccine. It is typically recommended that you wait 1-7 days between the biologic and COVID-19 injections.
Should people on allergen immunotherapy get the COVID-19 vaccine?
Yes, it is also safe for people taking allergen immunotherapy shots (for allergic asthma patients) to get the COVID-19 vaccine. It is not recommended that you take an allergen immunotherapy shot on the same day as the COVID-19 vaccine. It’s best to wait 4-7 days between the injections.
Reviewed by:
Purvi Parikh, MD, FACAAI is an adult and pediatric allergist and immunologist at Allergy and Asthma Associates of Murray Hill in New York City. She is on faculty as Clinical Assistant Professor in both departments of Medicine and Pediatrics at New York University School of Medicine.









