Vaccines for People with Asthma and Allergies
Published: August 30, 2024 Revised: February 13th, 2026

Do you or your child live with asthma, allergies, or another chronic lung condition? If so, you may face a higher risk of severe illness from contagious viruses like the flu. Even mild infections can make breathing harder, trigger asthma attacks, or worsen allergy symptoms.
Vaccines can help lower the risk of serious illness, hospitalization and death, while also supporting better lung health. Getting vaccinated is a personal choice, but it’s a good idea to talk with your healthcare provider about which vaccines are recommended for you or your child.
The following vaccines can help protect people with asthma and allergies:
- Influenza or flu vaccine
- COVID-19 vaccine
- Pneumococcal vaccine (for pneumonia)
- Respiratory syncytial virus (RSV) vaccine
- Whooping cough (pertussis)
Vaccines are available at doctor’s offices, health clinics and most pharmacies (including supermarket pharmacies). You do not have to get the vaccines all at once. However, if you so choose, you can get the flu, COVID-19 and RSV vaccines at one time.
Remember, no vaccine is 100% effective. Viruses – especially COVID-19 – can mutate quickly. Different versions of a virus can emerge. You may still get sick from a circulating virus even if you get vaccinated. If you do get sick, the vaccines can help prevent severe symptoms, hospitalization and death.
Need help finding where to get a vaccine? Visit the Champions for Vaccine Equity, Education and Progress website.
Learn the facts about vaccines for people with asthma and allergies. Here’s a breakdown of each vaccine:
Flu vaccine and asthma
The flu vaccine for the 2025-26 season is now available. It is once again a trivalent flu vaccine, typically delivered in one dose. The vaccine will protect against three main groups of circulating seasonal flu viruses: an A(H1N1) virus, an A(H3N2) virus, and a B/Victoria virus. The viruses in the vaccine are inactivated, meaning they cannot cause the flu.
People with asthma who get the flu are at higher risk for severe illness. Complications can arise even if asthma is well controlled. The flu virus can inflame the airways and trigger an asthma attack.
The U.S. Centers for Disease Control and Prevention (CDC) recommends all people 6 months of age or older, with rare exceptions, get the flu vaccine. It’s the best protection against getting sick with the flu and passing it on to others.
The U.S. Department of Health and Human Services (HHS) and the CDC recently updated the childhood immunization schedule. Parents of children who do not have health problems are now asked to talk with their child’s doctor before getting the flu shot. This is called clinical shared decision-making. Children with asthma are at higher risk for serious problems from the flu. Because of this, children with asthma should be able to get the flu vaccine without going through shared decision-making first.
You can obtain the flu vaccine as an injection or a nasal spray. It is available at most doctor’s offices and pharmacies. You can also obtain the nasal spray, called FluMist®, by mail delivery to your home. It’s the first flu vaccine available for self-administration at home. FluMist is approved for adults and children ages 2-49.
September and October are the best months for people to get vaccinated against the flu. This can provide protection for the entire flu season. But any time is better than not at all.
It’s important to note that the flu vaccine may vary in effectiveness year to year. It can depend on the match to circulating strains of the flu virus. However, even partial protection against the flu can reduce severity.
Remember, it takes about 2 weeks for the flu vaccine to provide protection after receiving the dose. Take that into account when you schedule your vaccine.
Most health insurance plans cover the annual flu shot as preventive care. Vaccination is often available at no or low cost to people who do not have insurance.
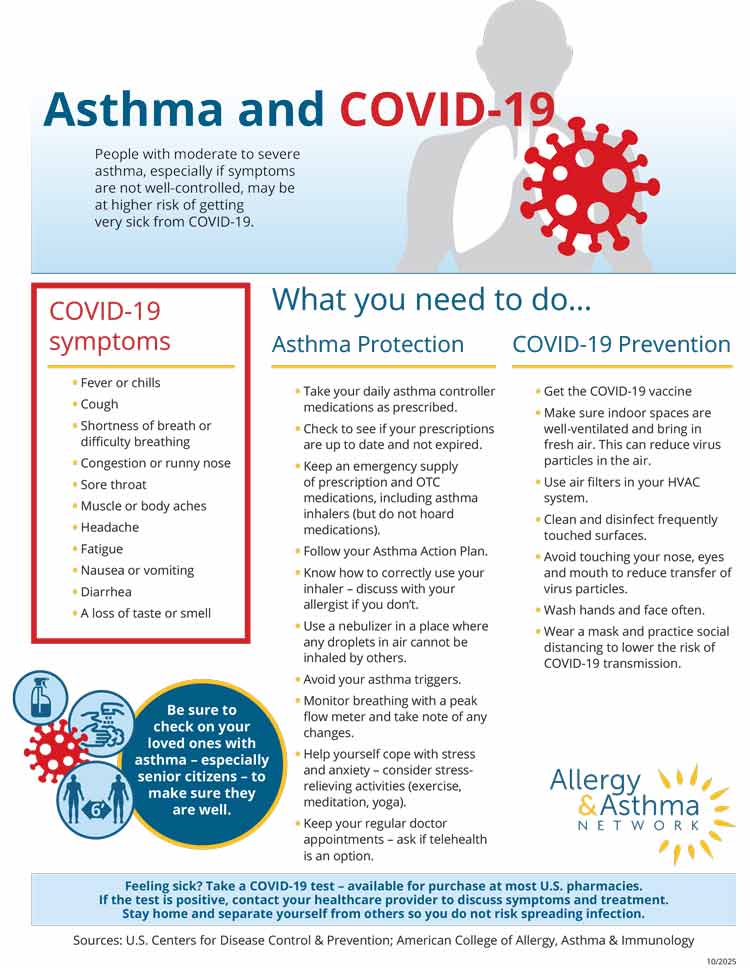
COVID-19 vaccine and asthma
The CDC has updated its COVID-19 vaccine guidance for 2025-26: all people 6 months of age and older, including adults 65 and older, are eligible to get the COVID-19 vaccine after consulting with a healthcare provider. (Healthcare providers include physicians, nurses and pharmacists.)
CDC says the consultation should involve clinical shared decision-making that focuses on the benefits and risks of the COVID-19 vaccine. According to a CDC advisory panel that reviews vaccines, the risk-benefit of COVID-19 vaccination is most favorable for people who have at least one high-risk health condition. This would put them at increased risk for severe COVID-19. The risk-benefit is lowest for people not at increased risk.
The U.S. Food and Drug Administration (FDA) approved age ranges for each of the available vaccines:
- Pfizer is available for adults and children ages 5 years and older. It is no longer available for children under 5 years of age. FDA removed the vaccine’s emergency use authorization (EUA) for that younger age group.
- Moderna is available for adults and children ages 6 months and older.
- Novavax is available for adults and children ages 12 years and older.
No prescription will be required to obtain a COVID-19 vaccine.
People with private or employer-based health insurance should check with their insurer to confirm the vaccine is covered. It will be fully covered under government programs such as Medicare, Medicaid, Children’s Health Insurance Program, Vaccines for Children Program, and insurance plans under the Affordable Care Act. Resources may also be available for people who are uninsured.
Some U.S. states are issuing COVID-19 vaccine guidance separate from CDC. Their guidance may make it easier for you to get the vaccine. Check with your state’s public health agency for information.
What health conditions put people at high-risk for severe COVID-19?
Before CDC updated its guidance to include everyone 6 months of age and older (subject to shared decision-making), FDA approved COVID-19 vaccines for people at higher risk of severe illness. This includes people with asthma, COPD and other long-term health conditions. (While FDA approves vaccines for use, CDC gives guidance on who should get the vaccine and how it should be used.)
The FDA list of health conditions that put people at elevated risk for severe COVID-19 illness (this is not a complete list and it may change):
- Moderate to severe asthma
- COPD
- Bronchiectasis
- Pulmonary hypertension
- Scarred lung tissue
- Cancer
- Diabetes (Type 1 or Type 2)
- Heart disease
- Being overweight or obese
- Mental health conditions including depression
- Physical inactivity
It’s recommended that people with one or more of these risk factors get the COVID-19 vaccine. For people with asthma, vaccination can reduce the risk of severe illness and help prevent an asthma attack.
Important reminder: People with asthma who get the COVID-19 vaccine should continue taking their medications as prescribed. This includes before and after receiving the vaccine. Keeping your asthma under control can reduce your risk of severe COVID-19 disease.
American Academy of Pediatrics COVID-19 Vaccine Recommendations
The American Academy of Pediatrics (AAP) has issued COVID-19 vaccine recommendations separate from FDA and CDC guidance.
AAP is recommending that parents of children ages 6 months to 2 years old get a single-dose COVID-19 vaccine for their child. AAP says this age group is at high risk for severe disease, hospitalization and death from COVID-19. For children ages 2-17, AAP is recommending to parents this group get the COVID-19 vaccine but it is optional.
AAP recommendations are supported by and aligned with several other medical organizations.
Download this infographic as a PDF
Pneumonia vaccine and asthma
Pneumonia is a serious, potentially life-threatening health concern for people with asthma. It is an infection that inflames air sacs in the lungs. People with asthma are at higher risk for more severe illness, complications, and hospitalizations if they develop pneumonia.
Pneumococcal pneumonia is the most common type of pneumonia – a bacterial lung infection caused by Streptococcus pneumoniae. It fills the lungs with fluid and pus, making breathing difficult.
The pneumonia vaccine protects against pneumococcal infections. CDC recommends the pneumococcal vaccine for:
- all adults 50 years of age and older
- adults ages 18-49 who are at risk for or have chronic lung diseases such as asthma or COPD
- children 5 years of age and younger (included as part of routine childhood vaccinations)
- children ages 5-17 who are at risk for or have chronic lung diseases such as asthma
The pneumonia vaccine is not an annual vaccine like the flu shot. It is either given as a single dose or a series of doses at certain ages or based on health conditions. Young children receive a 4-dose series, usually in the first two years of life. Some adults ages 65 and older may require multiple doses and/or a booster.
People with asthma who get the pneumonia vaccine should continue taking medications as prescribed. This includes before and after receiving the vaccine. Keeping your asthma under control can reduce your risk of pneumonia.
RSV vaccines and asthma
Three RSV vaccines are available for adults. The vaccines help develop antibodies against the protein that enters cells and causes RSV. The RSV season is typically September through April in the United States.
Abrysvo® and mRESVIA® are for adults ages 60 and older. They are also for people ages 18-59 who are at increased risk for lower respiratory tract disease (LRTD) caused by RSV.
Abrysvo is also available for pregnant people at 32-36 weeks of gestation during RSV season.
Arexvy® is another RSV vaccine for adults ages 60 and older. It’s also for people ages 50-59 who are at increased risk for LRTD caused by RSV.
In addition, a preventive RSV monoclonal antibody treatment called Beyfortus® is available for infants and young children. It works similar to a vaccine.
CDC recommends the RSV vaccine for:
- Adults over age 75
- Adults ages 50-74 who are at increased risk of severe RSV disease (this includes people with asthma)
- Pregnant people (Abrysvo only) at 32-36 weeks of gestation during RSV season
The RSV monoclonal antibody is recommended for all newborns and infants whose mothers did not receive the maternal RSV vaccine. Newborns and infants should be given the vaccine before experiencing their first RSV season (September to April).
The RSV monoclonal antibody is also recommended for children up to 2 years of age who are in their second RSV season and at high risk for severe RSV disease (this includes children with asthma or showing signs of asthma).
The RSV vaccine is not an annual vaccine like the flu shot. It is expected to provide protection for two years or longer.
Children who have severe RSV are at higher risk for developing asthma. Learn more about how to recognize the warning signs of RSV in children.
Whooping cough (pertussis) vaccines and asthma
Most children receive a series of whooping cough vaccines in their first year of life. They get boosters between 15 and 18 months and between 4 and 6 years of age.
Adults who have never had the whooping cough vaccine should get one. It is not an annual vaccine like the flu shot. Expectant mothers should get the whooping cough vaccine in the third trimester because it can help protect newborns.
People with asthma are at higher risk for getting whooping cough. They are also at risk for developing severe asthma symptoms if they do get whooping cough.
Measles vaccine and asthma
The measles, mumps and rubella (MMR) vaccine is typically given to children around age 1. Then children get a second dose before starting school.
Measles is a serious and potentially life-threatening disease, particularly for children under 5. It’s highly contagious and can lead to pneumonia and brain inflammation. About 1 to 3 of 1,000 measles cases can be fatal.
Measles can cause lung infections and worsen asthma symptoms. It can also weaken the immune system, increasing the risk of getting other illnesses.
The CDC recommends all children get vaccinated against measles (in addition to mumps and rubella). Adults who are not fully vaccinated against measles are urged to get caught up to stay protected.
The MMR vaccine is safe for people with asthma or allergies, according to the American College of Allergy, Asthma & Immunology (ACAAI).
Severe allergic reactions and vaccines
Severe allergic reactions to vaccines are very rare. If you or your child had a severe allergic reaction to a vaccine in the past, you should not get that vaccine. Talk with your healthcare provider about alternatives.
Allergic reactions to vaccines can occur in people who don’t have any known allergies. For this reason, It is recommended that all vaccines are given in settings where allergic reactions can be recognized and managed quickly.
People with egg allergy or latex allergy may have questions about vaccines based on their condition:
Egg allergy and flu/COVID-19 vaccines
Many people who are allergic to eggs express concern that vaccines have egg protein.
Some – but not all – flu vaccines contain egg protein. The amount is very small. CDC guidelines say flu vaccines do not pose a risk for an allergic reaction to eggs. So it is safe for people with egg allergy to receive the flu vaccine.
CDC has recommended that people with a severe egg allergy get the flu vaccine in a doctor’s office so they can be monitored afterward. But in 2023, CDC said this precaution is no longer necessary. If you are still concerned, ask your doctor about cell- or recombinant-based flu vaccines. These are egg-free and also available to the public.
COVID-19 vaccines are not made with egg proteins, so there is no egg allergy risk.
Latex allergy and vaccines
Some vaccines use vial closures and syringes that contain latex. There is concern that latex proteins may get mixed in with the vaccine. The risk level for a latex-allergic reaction to a vaccine is very low. You should receive your vaccines unless you have previously had a severe allergic reaction to latex.
When administering vaccines to latex-allergic people, healthcare providers can instead use:
- ampules that do not contain latex
- glass syringes
Healthcare providers should wear latex-free gloves when giving the vaccine. They should monitor patients with latex allergy after giving the injection.
Vaccines and pregnancy
Vaccines during pregnancy are crucial in preventing potentially serious diseases that can affect both the mother and the baby. For example, the flu can lead to severe complications during pregnancy, and pertussis can be life-threatening for newborns. Vaccination during pregnancy helps ensure that both mother and baby are protected.
Both the CDC and the American College of Obstetricians and Gynecologists (ACOG) recommend certain vaccines during pregnancy to safeguard maternal and infant health.
- Flu vaccine. Pregnant individuals are advised to receive the inactivated flu vaccine during flu season. CDC recommends pregnant individuals get a flu vaccine that is a single dose and free of thimerosal (a type of mercury) as a preservative.
- Tdap vaccine. This vaccine protects against tetanus, diphtheria and pertussis (whooping cough). It is recommended during each pregnancy, ideally between 27 and 36 weeks of gestation. This timing helps protect the newborn from pertussis in the early months of life.
- COVID-19 vaccine. Current vaccine guidance for pregnant people is unclear. In May 2025, CDC said it would no longer recommend COVID-19 vaccination for pregnancy. This decision was met with great concern from public health experts, including ACOG. However, in October 2025, CDC adopted recommendations that did not include specific guidance for pregnancy. Pregnancy is listed by CDC as a health condition that is high risk for severe COVID-19. So it’s expected that pregnant people will be eligible to get the COVID-19 vaccine – subject to undergoing clinical shared decision-making with a healthcare provider.
- RSV vaccine. This vaccine is recommended to protect newborns and infants from severe RSV disease. It can be given between between 32 and 36 weeks of pregnancy. The vaccine helps the mother develop antibodies that are passed on to the baby. It provides protection from severe RSV complications during the first six months of life.
The MMR (measles, mumps, rubella) and varicella (chickenpox) vaccines are not recommended during pregnancy. These should be given before or after pregnancy, as advised by a healthcare provider.
Talk with your healthcare provider about vaccination options so you can make informed decisions based on your health status and your specific pregnancy. Learn more about vaccines and pregnancy from CDC.
Questions & answers (Q&A) about vaccinations
Here are some frequently asked questions that patients ask doctors about vaccinations. If you have a question you would like to see added here, please email our editor.
Reviewed by:
Purvi Parikh, MD, FACAAI is an adult and pediatric allergist and immunologist at Allergy and Asthma Associates of Murray Hill in New York City. She is on faculty as Clinical Assistant Professor in both departments of Medicine and Pediatrics at New York University School of Medicine.









