
By Gary Fitzgerald
Ahh, germs. We’ve gotten to know them so well. Thanks to the coronavirus, we are all much more knowledgeable about bacteria, infections and how to avoid them than at this time last year when we were so blissfully unaware.
With no end in sight to the pandemic and the fall season bringing on the possibility of bacterial infections, not to mention cold viruses and the flu, there’s a greater sense of urgency this year to prevent them. (Wash your hands!)
It’s inevitable, though. Many of us will at some point come down with strep throat, a sinus infection, an ear infection and maybe even bacterial pneumonia. We will require antibiotics, including penicillin-based antibiotics such as amoxicillin, ampicillin and piperacillin.
What to do if you’re allergic to penicillin?
Hold on a second!
Are you absolutely sure you’re allergic to penicillin? How do you know for sure? Were you ever tested? No?
You could have penicillin allergy listed on your medical records and it could be completely wrong.
How Penicillin Allergy Mislabeling Happens
Penicillin allergy is the most commonly reported drug allergy in the United States. About 10% of the population report a penicillin allergy, but according to the American College of Allergy, Asthma & Immunology, more than 90% of those who think they are allergic to penicillin are actually not.
“That means at least 90% of people reporting a penicillin allergy are able to tolerate the antibiotic – because they likely never had a true penicillin allergy in the first place,” says Allison Ramsey, MD, a board-certified allergist and immunologist with Rochester Regional Health in Western New York.
Oftentimes the label of penicillin allergy is applied during childhood and carried on into adulthood.
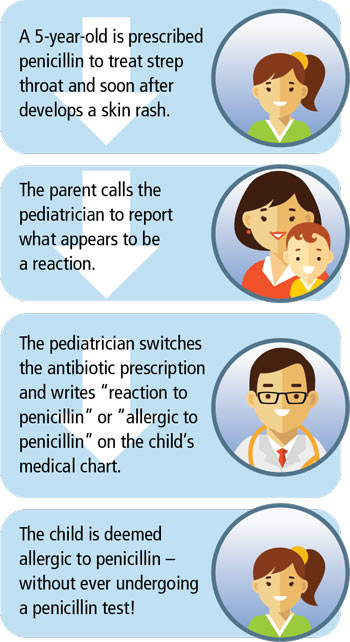
Here’s how the mislabeling can happen:
- A 5-year-old is prescribed penicillin to treat strep throat and soon after develops a skin rash.
- The parent calls the pediatrician to report what appears to be a reaction.
- The pediatrician switches the antibiotic prescription and writes “reaction to penicillin” or “allergic to penicillin” on the child’s medical chart.
- The child is deemed allergic to penicillin – without ever undergoing a penicillin test!
Many times the reaction the parent reported are not consistent with true allergy, according to research published in the Annals of Allergy, Asthma & Immunology.
Treating Bacterial Infections
Penicillin is the preferred antibiotic for bacterial infections because it treats the infection directly.
When you’re reported as having a penicillin allergy, your doctor may prescribe you nonpenicillin antibiotics to treat the bacterial infection. Nonpenicillin antibiotics may be less effective and involve more side effects and increased costs, Dr. Ramsey says.
Plus, you are increasing the risk of what’s called antimicrobial resistance. This occurs when bacteria changes in ways that make medications used to treat them ineffective. Using nonpenicillin antibiotics that treat a wide variety of illnesses could lead to drug-resistant bacteria – called “superbugs” – that increases risk of illness for everyone.
The most well-known “superbug” is methicillin-resistant Staphylococcus aureus (MRSA). Often found in hospitals, MRSA developed as a result of decades of often unnecessary antibiotic use. Simply put, germs that survived antibiotic treatment learned to resist others.
So as the season for bacterial infections arrives, you’ll want penicillin to be available to you for the infections that may come your way this fall and winter. If you think you or your child is allergic to penicillin, it’s important to get tested to find out for sure.
“If it’s determined you or your child are not truly allergic, then you can gain access to this important group of antibiotics,” Dr. Ramsey says.
Just think – you can free yourself of the burden of carrying a penicillin allergy label everywhere you go while also not enabling a potential “superbug.” A win-win.

Penicillin Allergy Testing is fast, accurate and safe
It’s simple. In a doctor’s office or hospital, you undergo a skin prick test in which the needle barely penetrates the surface of the skin. A raised, reddish wheal at the sight of the prick indicates a positive test for an allergy. No wheal, rash or hives? You’re probably not allergic after all.
Some doctors may follow up a negative skin prick test with an oral challenge – usually a full dose of liquid penicillin. The oral challenge has two purposes: 1) it confirms your negative test, and 2) it eases the fear factor over taking penicillin should you not be allergic. Again, this should only be conducted in a doctor’s office or hospital.
Here’s perhaps the best part of undergoing a penicillin allergy test: you get the results the same day. The process takes about 2 to 3 hours, including the time needed for doctors to monitor you for a reaction.
If it’s confirmed you or your child are not allergic to penicillin, there’s still one more step: remove the “allergic to penicillin” label on medical records.
Share the news far and wide. Tell your doctors, your dentist, pharmacies and schools and provide documents of the test results if necessary. Tell your family and friends.

A Note on Infections and Antibiotics
Antibiotics are only prescribed to treat bacterial infections, not viral infections such as COVID-19 or flu. However, if a virus weakens your immune system, common bacteria such as staph and strep can gain a foothold, possibly in the respiratory tract. This can lead to sinus infections, ear infections or pneumonia that would then require antibiotic treatment.

 810304 Eaton Place, Suite 100
810304 Eaton Place, Suite 100